Why Americans and Europeans may soon start dying of infections like it’s 1905 again
Antibiotics aren’t doing what they’re supposed to do anymore. You know, kill infections. Since Alexander Fleming invented penicillin 75 years ago, nearly all bacteria have mutated into strains impervious to antibiotics. Those souped up bacteria now kill hundreds of thousands of people, at a minimum, each year. And according to a new issue of medical journal The Lancet focused on antibiotic-resistant bacteria, things could soon get a whole lot scarier.
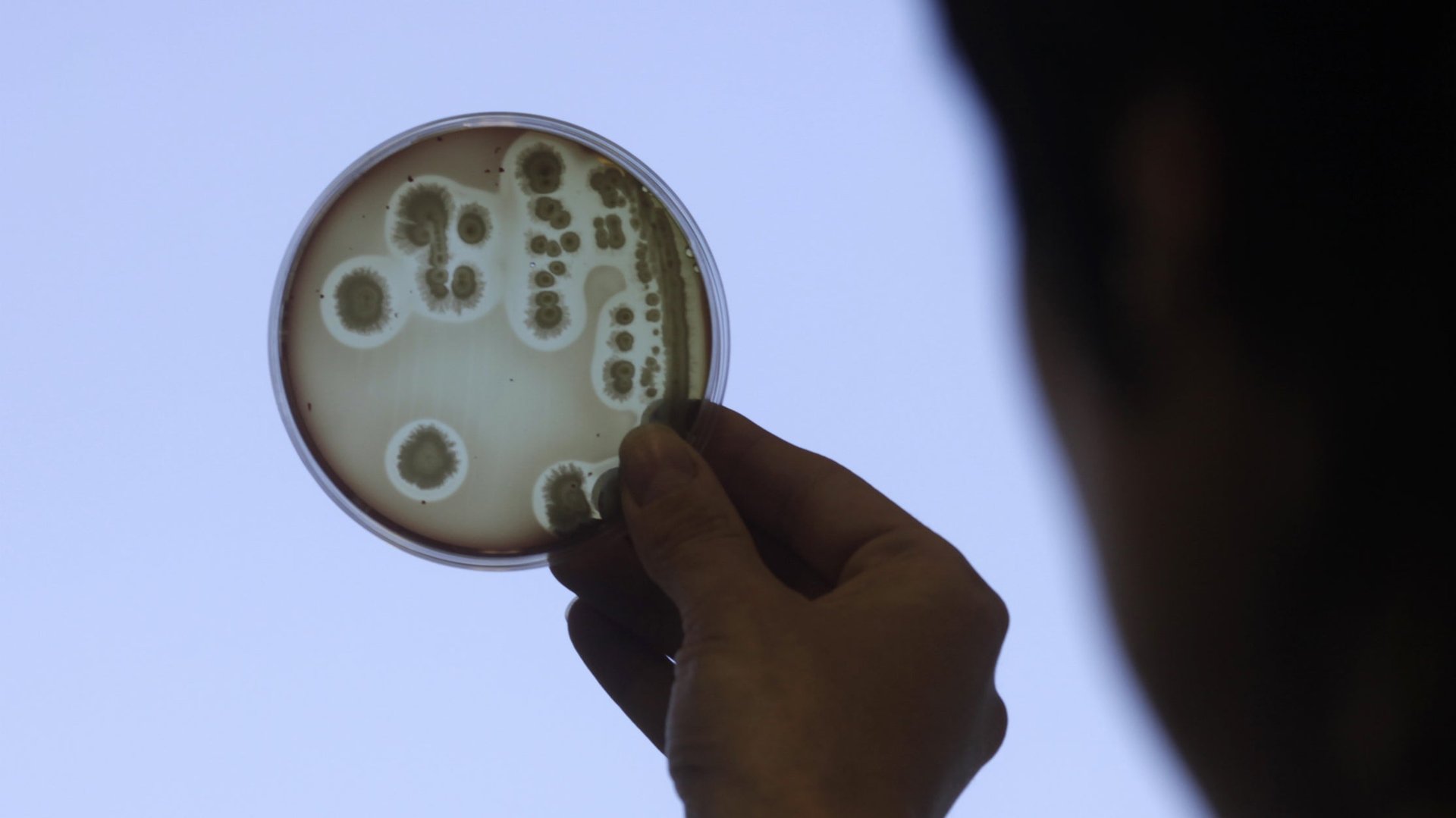
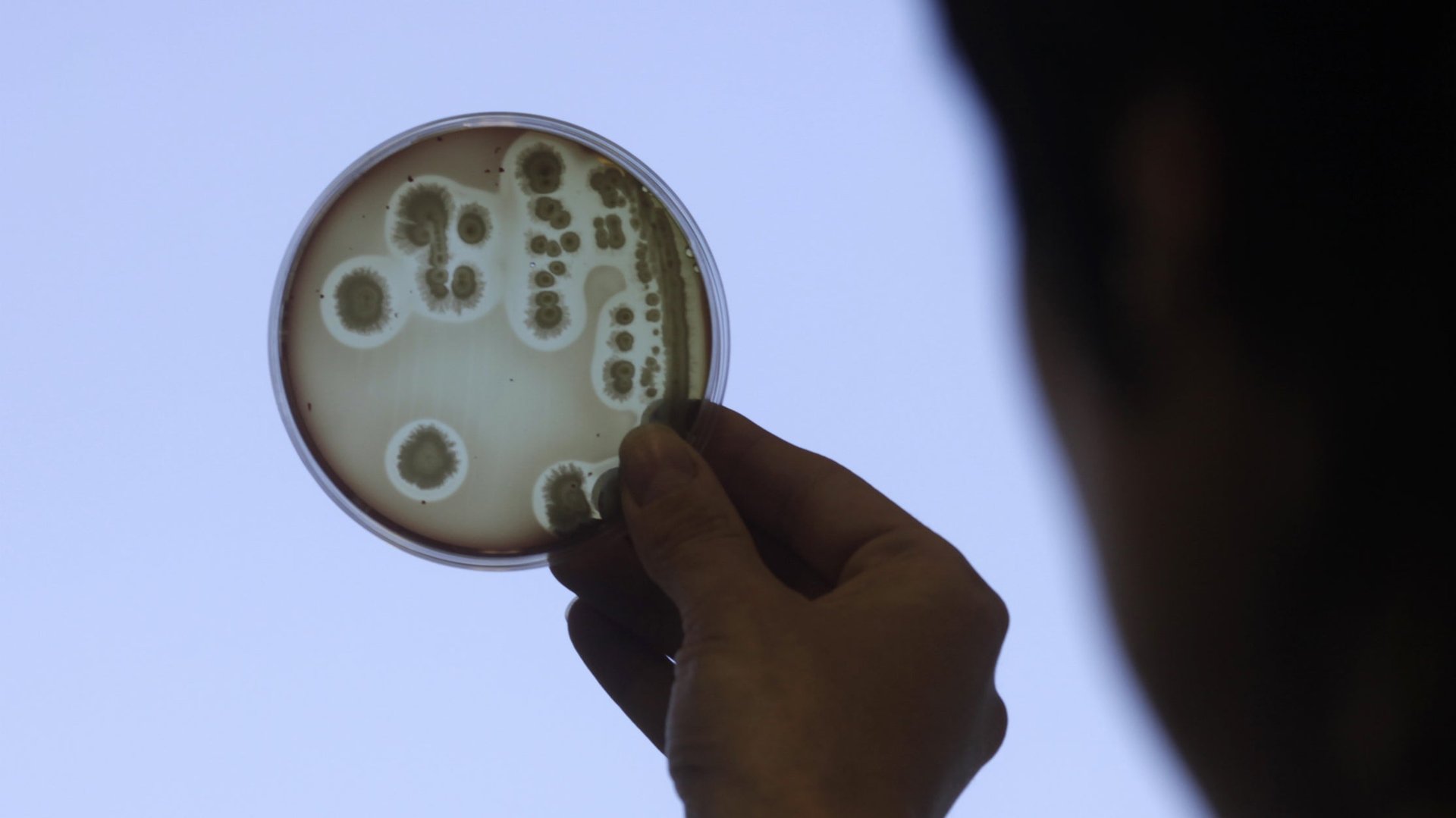
Antibiotics aren’t doing what they’re supposed to do anymore. You know, kill infections. Since Alexander Fleming invented penicillin 75 years ago, nearly all bacteria have mutated into strains impervious to antibiotics. Those souped up bacteria now kill hundreds of thousands of people, at a minimum, each year. And according to a new issue of medical journal The Lancet focused on antibiotic-resistant bacteria, things could soon get a whole lot scarier.
“Rarely has modern medicine faced such a grave threat. Without antibiotics, treatments for minor surgery to major transplants could become impossible…,” argue a team of UK medical experts in one article in a series on antibiotic resistance (paywall) in The Lancet. ”Infection-related mortality rates in developed countries might return to those of the early 20th century,” they say.
The reason antibiotics are no longer doing what they’re supposed to is mainly that they’re being given to the wrong patient. Instead of people with severe infections or risk of infection, the majority of antibiotics are consumed by animals and people who aren’t sick enough to justify their use.
Pigs, chickens, cows, fish and other animals consume the majority of the 100,000-200,000 tonnes (110,000-220,000 tons) of antibiotics manufactured each year, as farmers try to keep growing large and healthy animals under unsanitary conditions. The bacterial strains created in these conditions can spread to humans.
At the same time, perverse incentives in poor countries encourage overuse. People often take antibiotics available over-the-counter, says The Lancet’s report on global resistance, and self-medication by consumers is common. The lack of sound medical care in some areas means that pharmaceutical companies are the chief source of information on when to take antibiotics and in what dose.
Meanwhile, financial kickbacks in India and China spur overprescription. The Lancet cites one study showing that antibiotics sales generated one-quarter of revenue from two Chinese hospitals. That explains why the average Chinese person takes 10 times more antibiotics than the average US patient does.
Even in the US and other rich countries, health care systems commonly overprescribe antibiotics for upper respiratory infections, says The Lancet report.
The more people and animals consume antibiotics—and the more they do so in an uncontrolled way—the greater the likelihood of generating resistant bacteria, or “superbugs,” as they’re often called.
People who need them aren’t getting them. More than 25% of the 6.6 million children who died before the age of five in 2012 succumbed to preventable infectious diseases like pneumonia and infant sepsis, according to another article (paywall) in The Lancet. For parents of some of these babies, the prices of fancier antibiotics—drugs that are able to fight these bacteria—are far out of reach.
What can be done? There are two obvious starting places. Use of antibiotics among animals, except in therapeutic situations, must end, says the report. It also recommends that in all but the poorest countries, over-the-counter sales of antibiotics must be banned. We also need pharmaceutical companies to develop more antibiotics, though that will take time.
And that’s just a start, says Dr. Otto Cars, a professor at Uppsala University and lead author of The Lancet report. “Addressing these problems will require nothing less than a fundamental shift in how antibiotics are developed, financed and prescribed,” Cars says.