There’s nothing rational about deciding who lives and who dies
America has finally entered an era of universal medical coverage. ObamaCare, as the Affordable Care Act is colloquially known, will necessitate difficult decisions relative to the dissemination of the medications and procedures required by people to stay healthy and fight illness. In other words, Americans will need to get used to the idea of healthcare rationing.
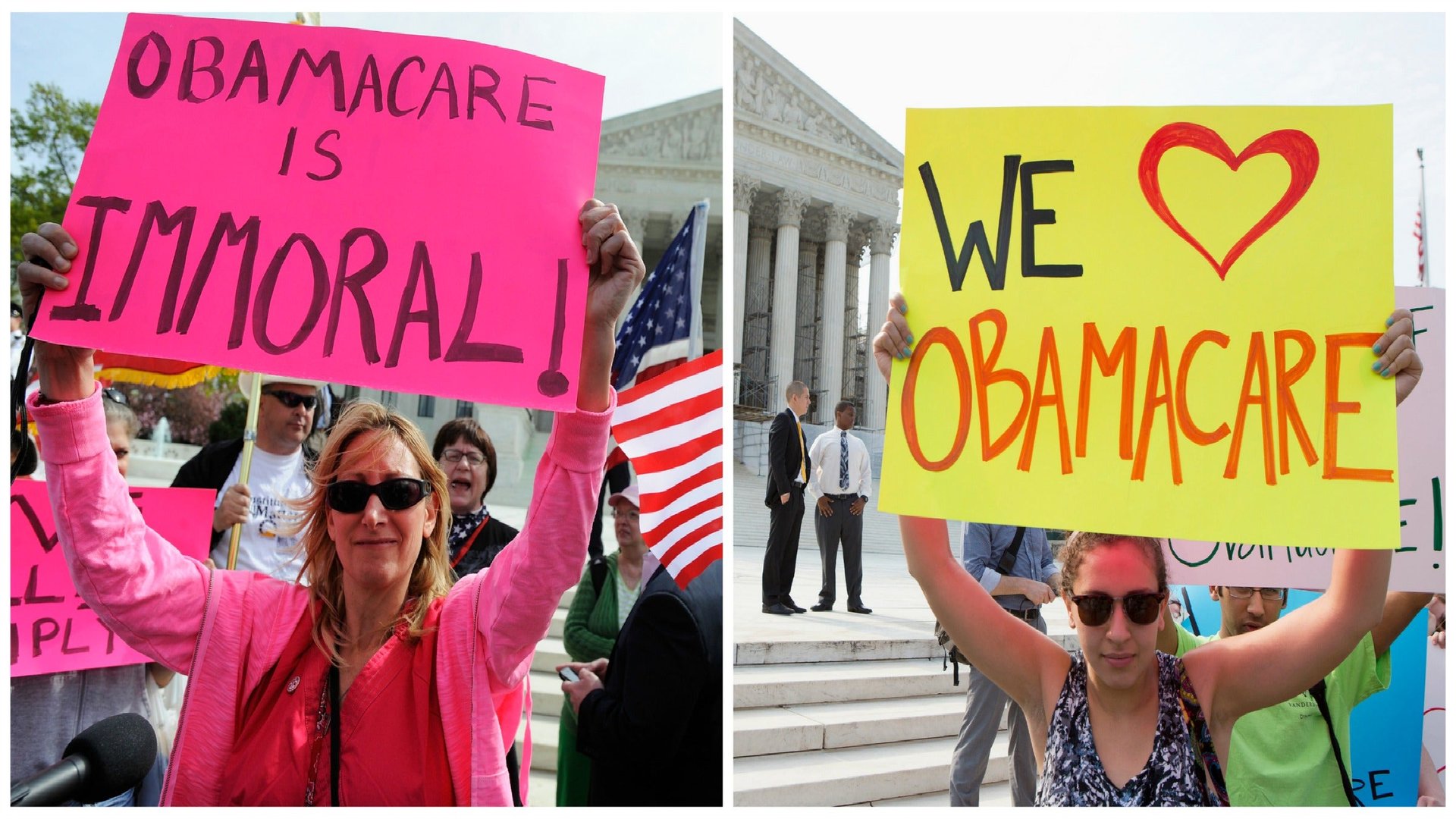
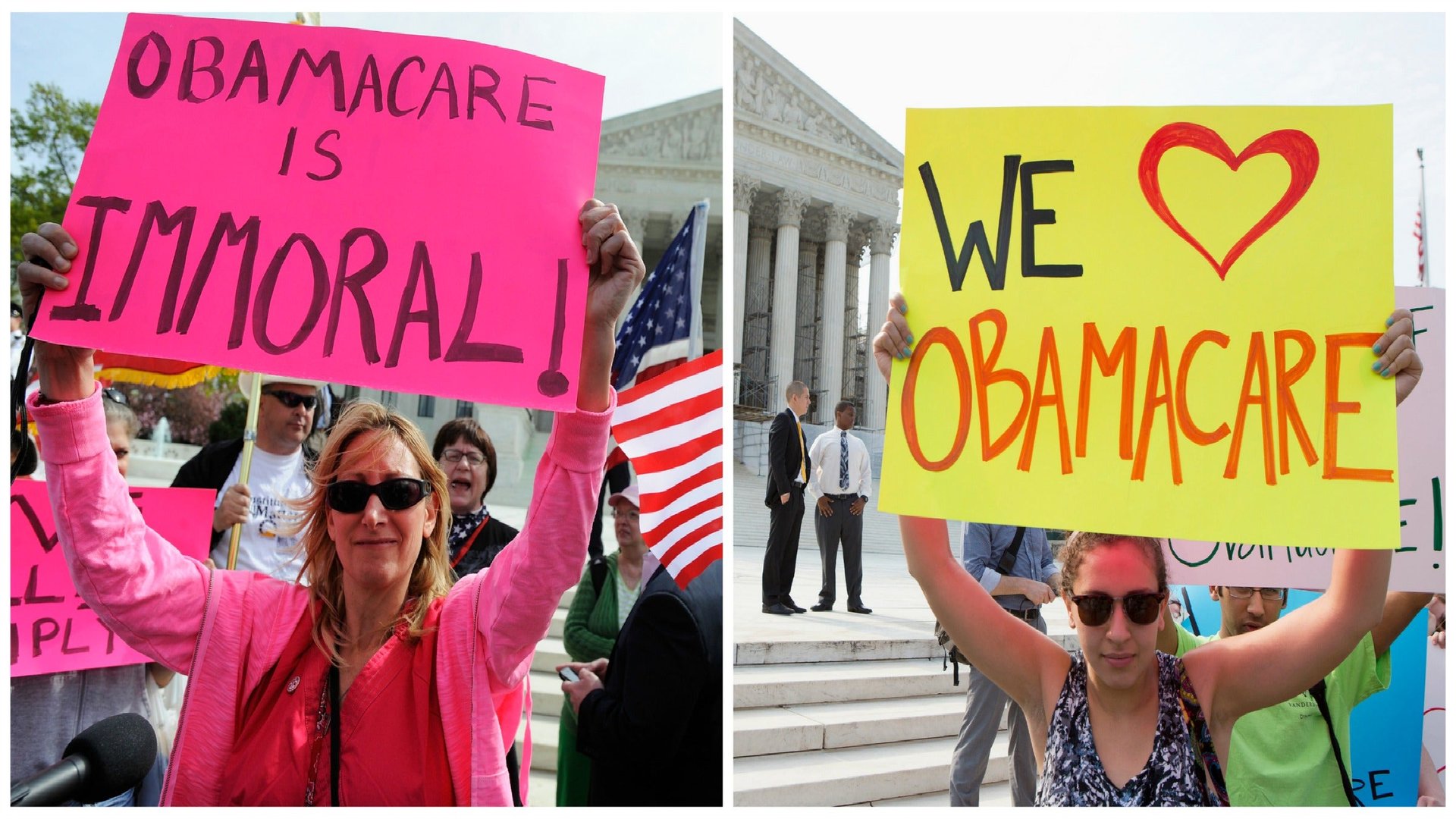
America has finally entered an era of universal medical coverage. ObamaCare, as the Affordable Care Act is colloquially known, will necessitate difficult decisions relative to the dissemination of the medications and procedures required by people to stay healthy and fight illness. In other words, Americans will need to get used to the idea of healthcare rationing.
As economic policy, rationing is the restricted allocation of scarce resources, generally through government oversight. In its most altruistic form, it reflects a process of collective sacrifice for a collective good, such as restrictions on rubber products to promote the American military effort in the 1940s. Sometimes it is simply a matter of expediency, as in the limits on gasoline sales in New York City to avoid customer frustration at the pumps and gnarled traffic after Superstorm Sandy. In these instances, rationing is transparent, equitable, and non life-threatening, the resultant public grousing is limited, and life quickly moves on. Health-care rationing, however, is frequently neither transparent nor equitable, and can be profoundly life-threatening in ways both subtle and heart-wrenching.
This summer, the case of Sarah Murnaghan, a 10-year-old girl from Pennsylvania diagnosed with cystic fibrosis, ignited controversy around the issue. Sarah’s parents succeeded in stimulating public discourse about what became known as “the Under 12 Rule,” code for offering available adult lungs to adult patients and correspondingly matching pediatric patients with organs harvested from other children. But armed with thousands of signatures from a Change.org petition, and a temporary restraining order from a federal district court, Sarah’s parents prevailed upon US Health and Human Services Secretary Kathleen Sebelius as well as the Organ Procurement and Transplantation Network (OPTN) to create a mechanism for individualized, case-dependent exceptions to the aforementioned rule.
As expected, the debate and subsequent ruling generated strong opinions on both sides of the issue. In some instances, the responses followed party lines. The House GOP Doctor’s Caucus, writing as “both medical professionals and lawmakers,” opined that the current OPTN age policies were discriminatory and respectfully asked Secretary Sebelius in advance of the court ruling to suspend the “Under 12 Rule” under review. Senator Robert Casey, acting on behalf of his constituent, similarly implored the OPTN for a timely policy review. Sarah Palin was considerably less charitable, and less muted, resurrecting her “death panel” charges and leveling them at Secretary Sebelius and HHS. On the opposing side, Alexandra Glazier, ethics committee chair of the United Network for Organ Sharing (UNOS), voiced concern that involving the judiciary in such matters invites “significant chaos and inherent unfairness because access to the courts is not equal.” Finally, transplant medical experts were nearly unanimous in their support of the current system, summarized by Dr. Stuart Sweet’s comments, a board member of UNOS, “We’ve built a system that tries to be as fair to everyone as possible…it’s the best we can do right now.”
Cystic fibrosis (CF) is a recessive genetic condition. When diagnosed during childhood, it is uniformly fatal by the time you hit your forties. The downward spiral is caused by repeated lung infections, and life becomes increasingly constrained by lengthy home treatments to clear plugged airways, frequent emergency room visits, and prolonged hospitalizations. There is no cure for CF, and the only long-term treatment option is lung transplantation.
It seems that Sarah’s course deteriorated when thick, sticky mucus accumulated in the lungs causing pulmonary failure. As such, a lung transplant was sought. Sarah ultimately qualified to receive organs from adult donors. On June 12, the first transplant failed, but three days later a second transplant (with lung tissue known to be infected) was rapidly carried out in view of the tenuous clinical situation. The post-operative course has been complicated and at this writing there is still prognostic uncertainty, but all are rooting for Sarah’s recovery.
Human organs are among the most precious and rare of societal commodities, and as with all limited resources, their allocation must be thoughtfully regulated. However with lives hanging in the balance, distributing a heart or lung is not the same as the economics 101 conundrum of manufacturing guns or butter. Sarah’s plight places a very human face on the ethical dilemma of whether the benefits of organ transplantation justify the expense, and just as we learned in elementary economics courses, there is an “opportunity cost” for these decisions. The direct and indirect costs of a lung transplant in the first post-operative year approach $500,000; the cost of a flu vaccine is less than $10. Money spent on aggressively immunizing our elderly and infirm would undoubtedly save more lives than transplanting a single lung, but who among us would express this position to the Murnaghans? Indeed, who among us would listen to this argument if it were our own child dying of cystic fibrosis?
Beyond these economic concerns, organ donation in very practical terms is a zero sum game. Because Sarah Murnaghan received a lung transplant, someone else on the lung transplant list is still awaiting his or her turn. Since there are not enough organs to fill the needs of terminally ill patients with chronic lung disease, that nameless individual may not be as fortunate as Sarah to have a chance for long-term survival. Indeed, each year approximately 400 patients die awaiting a lung transplant in the United States. Until recently, lungs were distributed based on the length of time one was listed for the organ: a “first come, first served” approach. At present, urgency of need has been added to the algorithm, and trumps length of illness. That Sarah was deemed eligible for an adult organ speaks to the medical rationale that her youth did not substantially reduce the likelihood of a successful outcome. The same cannot be said of the other end of the spectrum, as lung transplant centers frequently will not provide an organ to those over age 65. Yet is it fair to deny a healthy 67-year-old with chronic lung disease a lung transplant, but to offer the organ instead to a 62-year-old with medical illnesses like heart disease or diabetes, who may be less apt to survive the rigors of the procedure?
The Organ Procurement and Transplantation Network does not think so, and has crafted organ-specific allocation rules that incorporate this philosophy. For lung transplantation, a lung allocation score is calculated for every potential adult recipient. It is based on the difference between the number of days a transplant candidate is expected to survive during the first year post-transplant and the expected number of days a candidate will live without a transplant during an additional year on the waiting list. This is a complex calculation that encompasses over 20 variables including age; however, age alone is not a disqualifying factor. Absent from the calculation is a measure of the expected long-term benefit of lung transplant recipients. Indeed, in a 2009 analysis of UNOS data, younger CF patients (age under 20) were 19% less likely to be alive 5 years after transplant than older patients (age over 35), negating an argument that younger CF transplant recipients are more likely to enjoy multiple years of benefit following lung transplantation. By this reckoning, Sarah’s youth should not work in her favor in procuring an organ, and older candidates should not be penalized by the process.
But is this process working? From Sarah’s perspective, the answer was a resounding no. As with all rationing systems, lung allocation strategies benefit some and deny others, and declaring whether the process works is an exercise in relativity. A better question is whether the current system adequately balances the conflicting goals that are inherent in all rationing systems. While all may agree that transplanted organs should be provided to those most in need, reasonable minds will differ when determining whose claims are most meritorious. How should one balance wait time on a transplant list, severity of illness, likelihood of benefit, tissue compatibility of donor and recipient, adequacy of recipient support systems, and a host of other factors that would speak to this question? Eric Cohen, writing for the President’s Council on Bioethics on transplant allocation strategies in 2006, eloquently stated the dilemma. “We need a thoroughly rationalized system that gives each potential recipient a rank on the list, and yet the rankings always require imperfect clinical judgements, as well as spot decisions by doctors, decisions made under pressure, with inadequate time, always open to second-guessing by others, both in the moment and after the fact. We thus need to improve and refine the system, while recognizing the permanent limits of the system.”
The Murnaghans acted nobly as parents, challenging the OPTN for the first time in court, but some would argue that society cannot operate without striving to deliver the largest possible benefit for the greatest number of people. Nonetheless, in implementing a utilitarian principle, one of the charges frequently lobbed in chat rooms and blogs was that a little girl’s life was hanging in the balance as “doctors were playing god.”
Ask a patient and you are likely to be told that this is the underlying expectation of a physician who is continually asked to make “life-and death decisions” and who feels entitled, given her level of education and experience. Many physicians, on the other hand, will assert that patients themselves deify the profession and that it is a form of wistful longing: “If my doctor really is god-like”, the thinking goes, “then mistakes won’t be made and cure will be achieved.”
Other than battlefield triage choices or hospital evacuation decisions during environmental catastrophes, the reality is that doctors rarely make life-or-death decisions. While physicians are often privy to the goings-on of the decision-making process, it may be surprising to note how infrequently they are actually the primary decision-makers. In the Murnaghan case, Sarah’s pediatricians as well as her pulmonologist were enlisted to seek a suitable transplant and they, too, were willing to challenge the guidelines of HHS. Physicians involved in patient care are analogous to defense attorneys in a courtroom. Just as every defendant is entitled to a spirited defense, every patient deserves a vocal physician advocate whose primary concern is providing optimal care and achieving an optimal outcome. And just as defense attorneys are not also judge and jury, individual physicians are not the final arbiters in all clinical matters.
With regard to organ transplantation, the distribution of human organs is governed by federal statute. In 2000, the Final Rule clarification of the National Organ Transplant Act empowered the OPTN to establish uniform organ transplantation guidelines and stipulated the governance of this body. By law, approximately half of the OPTN Board of Directors must be transplant surgeons or transplant physicians, and at least 25% must be transplant candidates, transplant recipients, organ donors and family members. Of note, these members “should represent the diversity of the population of transplant candidates….served by the OPTN,” and reflect, “to the extent practicable, the minority and gender diversity of this population.” Not only were the Murnaghans likely to have a sympathetic audience to hear their case, but the National Organ Transplant Act granted them direct appeal to a powerful arbiter, the Director of Health and Human Services.
However upon initial review, Secretary Sibelius asked only for an investigation of the fairness of the “Under 12 Rule,” which mandated that children under 12 be assigned first priority for pediatric donor lungs, second priority for adolescent donor organs (ages 12-17), and tertiary consideration for available adult lungs. As Sarah was not likely to survive pending a detailed evaluation of the appropriateness of this algorithm, her parents took the case to federal court, and obtained a temporary restraining order. Compelled by the court ruling and the media hailstorm that followed, the OPTN then decided to allow a waiver of the “Under 12 Rule” in select cases, enabling Sarah and a second child to receive adult lungs, while mandating further study. A final decision on whether to maintain the “Under 12 Rule” in its current form or to allow children equal access to adult donor lungs is expected by July 2014.
Experts ranging from physicians to ethicists to the legal community have voiced strident opinions about both the outcome and the process of this case. Writing in the Annals of Internal Medicine, Dr. Scott Halpern, a physician and bioethicist from the University of Pennsylvania, described the intervention of the court as setting “a troubling precedent.” Halpern expressed concern that “the court did not seek evidence to assess the merit of the age-discrimination claim,” and that “the court’s response exalted [Sarah Murngahan] and another child above a national policy, suggesting either failure to recognize that preferential treatment for some recipients will adversely affect others…or that the court considered these two children’s lives more valuable than others’.” In reply, Stephen Harvey, lead counsel for the plaintiffs in the federal suit, claimed that his clients “asked only that they be given access to adult lungs based on the medical urgency of their conditions,” and that the plaintiffs “be treated equally with persons over 12 absent some compelling reason to do otherwise.”
In the complaint brought before federal court, Harvey provided some sobering statistics. Between 2009 and 2011, the complaint alleged that the average death rate for children awaiting a lung was 46%, versus 28% for adults. In 2011 data from UNOS summarized in the complaint, the rate at which adults on the transplant list received a lung was 50%, compared with 30% for the pediatric population. While an age discrepancy in lung transplant statistics does not in itself prove an age discrimination bias, the numbers seem sufficiently alarming to merit scrupulous review.
Dr. John Roberts, president of the Board of OPTN, supported the current system in a letter advising Secretary Sebelius prior to the filing of the court case. Roberts highlighted the scarcity of data for transplant outcomes in the pediatric age group (approximately 20 pre-adolescent transplants are performed in the US annually, versus over 1600 adults), and the substantial differences in lung diseases leading to organ failure in children versus adults, as qualitative arguments in favor of the “Under 12 Rule.” Though these facts may justify a separate allocation scheme for the pediatric population compared with adults, they do not confirm that this separate paradigm provides an equal benefit. Conspicuously absent from the pretrial public record is a statistically valid defense of the rule, either supporting its creation in 2005 or confirming its validity in 2013.
Absent concrete evidence to justify the “Under 12 Rule,” guided by a federal mandate to “recognize the differences in health and in organ transplantation issues between children and adults throughout the system and adopt criteria, policies, and procedures that address the unique health care needs of children,” and with the life of a child hanging in the balance, District Court Judge Michael Baylson issued the temporary restraining order on June 5, 2013, pending a formal injunction hearing 10 days later. At a June 10th executive OPTN meeting, a detailed statistical review of wait times, transplant rates, and death rates, grouped by patient age and covering the period between 2010 and 2013, was presented. It found no significant age bias in the current allocation scheme, but rather than defend this position at the scheduled injunction hearing, the OPTN opted instead to define a waiver process for the “Under 12 Rule” in select circumstances pending further study of the rule. Halpern voiced disappointment with the “legal and political leaders who neglected their responsibility to protect the interests of all potential patients,” yet Baylson can hardly be faulted for his decision when the OPTN itself expressed doubt with the “Under 12 Rule” in spite of its own statistical analysis.
As much as we would hope that ethical decision-making is a black and white process, it is a gross simplification to label rationing strategies such as organ allocations as right or wrong. They are best viewed as complex balancing acts, with crafters walking a tightrope between individual rights and societal needs. Sometimes, given the emotional angst that accompanies difficult decisions like the Murnaghan case, the tightrope is more like a high-tension wire. The “Under 12 Rule” was crafted in 2005 with the goal of benefiting children, not harming them. It was devised with the thought that pediatric patents fared better with pediatric donor organs, but that given the limited availability of such organs children should have secondary access to adult donor organs. Of note, to strengthen the pediatric odds, adults were not granted reciprocal access to pediatric organs. If the OPTN’s final review indicates that parity has not yet been achieved between pediatric and adult transplant candidates, this is not an indictment that the “Under 12 Rule” was misguided at its inception. Rather it is an inducement to revisit policies initially formulated with incomplete data, and reformulate them under the clarity of scientific hindsight to make them better.
A real concern raised by the Murnaghan case is that a precedent has been set for lower priority transplant candidates to resort to court intervention to bypass carefully-crafted allocation guidelines, and enhance their standing. This is a misreading of the outcome of the Murnaghan case; as Sarah’s goal was to achieve equal ranking with adults on the transplant list, not preferential treatment. In addition, her suit did not challenge a transplant criterion already determined to be valid by exhaustive scientific review, such as the LAS score as used in adults, but a factor—age—whose inclusion in the lung transplant algorithm was based on a less secure foundation. Current organ allocation guidelines reflect a mix of scientific fact, expert opinion, and public health incentives designed to motivate individual behavior to promote a societal good. No doubt some of these factors will be subject to future challenge in the courts; however as Harvey stated, “the possibility of baseless claims is not a reason to reject meritorious claims.” Two strategies should be considered to reduce the likelihood of frivolous suits. First, mandate inclusion of a wide array of experts on the OPTN Board, to include ethicists, health care economists, game theorists and legal experts, such that future allocation strategies are vetted broadly before implementation and less prone to dispute. Second, require that an expert review panel, similarly but independently configured, evaluate the validity of challenges to the current law, and determine whether a suit has sufficient merit to move through the courts.
In contrast to the Murnaghan case, an illustrative example of failure to deliver optimal treatment due to market forces with a more opaque and less representative appeal process occurred overseas. In Israel, where national health care legislation has been available in some form since the founding of the state in 1948, a committee meets annually to revise the “basket” of medical goods and services that are provided to all citizens. Unfortunately, the basket often lags behind the establishment of new standards of care. In 2005, a study appeared in the prestigious New England Journal of Medicine which established a new treatment paradigm for the most aggressive type of brain tumor (glioblastoma multiforme or GBM). Swiss investigators proved conclusively that instead of treating with radiotherapy alone, the combination of radiotherapy and a drug known as temozolomide nearly doubled survival rates. The drug, manufactured then by Schering Plough, was priced at approximately 40,000 sheqels (approximately $10,000 USD in 2005) per month and was to be taken for a full year. Temozolomide was not added to the aforementioned basket for nearly two years. Israeli citizens diagnosed with GBM who could not afford to pay the $120,000 to acquire the drug had no clear recourse.
As many of the Israeli patients were savvy medical consumers, a creative solution emerged. Israelis obtained access to a clinical trial sponsored by the National Cancer Institute which randomized patients diagnosed with GBM to irradiation plus standard-dose temozolomide versus irradiation plus dose-intensified temozolomide. In both the standard arm and the experimental arm of the study, patients received the drug gratis from the NCI. Israel became the leading accruer of patients to this study, outpacing highly regarded academic centers in the US such as MD Anderson Cancer Center in Houston and Harvard University. But what of those patients with GBM who did not meet “eligibility criteria” (based on laboratory tests or other picayune factors that might exclude someone from enrolling) to gain access to the study? And do we know that those who were admitted to the study went through a valid process of “informed consent” or were these patients unlikely to carefully weigh the potential downsides of entering the study having been overcome by their motivation to obtain free temozolomide? Of note, in the ensuing period temozolomide was inserted in the Israeli health basket and subsequent clinical trials designed to study GBM had much lower representation by Israeli patients.
In explaining the decision of the committee presiding over the health basket to delay the inclusion of temozolomide, an anonymous committee member implied that a tough decision had to be made to forego the life-extending drug for the few patients diagnosed with brain tumors to allow inclusion of other drugs for common, benign diseases. “It’s a closed system,” he remarked, “so when you squeeze the air from one region, the pinch is felt in other parts of the balloon.”
Indeed, the pinch will invariably be felt by someone. But will Americans, raised in a tradition of fairness that disdains inequity, yet immersed in a culture of entitlement at any cost, be able to come to terms with the pinch? The ACA is a move toward providing universal healthcare coverage, not universal access to all aspects of health care. Will we at least be able to take solace in the silver lining of rationing? Specifically, guidelines established in anticipation of cases such as Sarah Murnaghan’s, if nothing else, indicate that the appeals process can be not only rational but also empathic. With the growth of costly medical treatments and a range of impassioned stakeholder opinions, rational health care rationing is undoubtedly a moving target, but at least all can agree it is a goal worth aiming for.