Every expert opinion you’ve heard about wearing masks is right
[Update 4/3/20: Yes, you should wear a mask. The US Centers for Disease Control and Prevention is now recommending everyone wear a mask “in public settings where other social distancing measures are difficult to maintain,” such as grocery stores, to slow the virus’s spread. The type of masks it’s apparently ready to recommend are cloth masks made from common fabrics such as cotton. More effective N95 respirators and surgical masks, which use specialized textiles, would continue to be reserved for healthcare workers and first responders. They’re already in critically short supply with the US unable to meet demand for those most in need, let alone the general public.]


[Update 4/3/20: Yes, you should wear a mask. The US Centers for Disease Control and Prevention is now recommending everyone wear a mask “in public settings where other social distancing measures are difficult to maintain,” such as grocery stores, to slow the virus’s spread. The type of masks it’s apparently ready to recommend are cloth masks made from common fabrics such as cotton. More effective N95 respirators and surgical masks, which use specialized textiles, would continue to be reserved for healthcare workers and first responders. They’re already in critically short supply with the US unable to meet demand for those most in need, let alone the general public.]
Should you wear a mask to stop the coronavirus? It’s a fraught question. Depending on where you live, the act risks social censure, accusations of selfishness, and perhaps the infection itself. No one wants to say they don’t know.
Asking eight health authorities will elicit eight different answers. A brief review of health agencies’ recommendations for the coronavirus from around the world adds to the confusion. In China, the government has told almost everyone to wear disposable masks (and sometimes mandated it). In Japan and Hong Kong, anyone entering crowded places are asked to don them. In the West, the message is the opposite. Germany’s Federal Ministry of Health warns mask wearers risk lulling themselves into a “false sense of security.” America’s top health official, battling a catastrophic shortage of masks for healthcare workers, has tweeted for people to “STOP BUYING MASKS! They are NOT effective in preventing the general public from catching #Coronavirus.”
For the public, the situation is maddening. In the US, officials appear to be managing scarcity rather than speaking honestly about masks’ effectiveness. In Asia, public health officials call it “common sense” and even designed homemade versions for people to fashion from paper towels. Researchers who see no evidence for their effectiveness in the general population, when pressed, will take a deep breath and admit wearing masks themselves.
What can scientists say with certainty? The literature is unequivocal on one point: Masks protect healthcare workers from high levels of viral pathogens. From the lowly paper mask to ultra-high filtration N95 masks designed to stop aerosols, decades of studies show masks stop healthcare workers from getting infected in hospitals, and prevent sick people from spreading disease to others.
As for whether everyone should wear a mask to slow a pandemic, the answer is far less clear.
Epidemiologists cannot point to any conclusive evidence after years of studies. Almost all the research suffers from small sample sizes or confounding variables that distort results. “It’s all a little mysterious, but that’s science for you,” says Andrew Noymer, a public health professor at the University of California Irvine. “People look to science for really crisp advice. Scientists often spend their lives arguing with each other about shades of grey.”
That argument is now about saving lives.
What we know for sure
The coronavirus, like influenza and other viruses, spreads through the diffusion of millions of tiny viral particles. After someone coughs, sneezes, or touches an object, these particles can settle on a surface or hang briefly in the air, primarily in droplets. Viral particles, as many as tens of thousand per droplet, can gain access through our nose, mouth, or eyes after we touch our face or breathe while in close contact with someone who is contagious. If the dose is high enough—and a single droplet may do it—the virus can replicate in our body, starting the infection cycle again.
Almost every version of manufactured masks, from every day surgical masks to N95 respirators appear to confer at least some level of protection against this transmission. Study after study has confirmed that in hospitals. 1

Masks can work at home as well. Both the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC) advise mask use for people caring for those with Covid-19, as well as those infected.
But this is where the evidence becomes less clear. One 2009 CDC study showed masks could cut caretakers’ risk of viral infection by 60% to 80%—but less than half of people in the study wore their masks consistently. Some other studies have noted no effects within households.
At a population scale, the impacts of mask usage are still murkier. One of the largest attempts to measure mask efficacy was at the University of Michigan during the 2007–2008 influenza season. Researchers divided 1,178 students into three groups: One group was asked to wear face masks at least six hours per day in their dorm, a second received masks plus hand sanitizer, and a third served as controls. While hand sanitizer appeared to have an effect, it wasn’t statistically significant, and masks alone showed no effect at all. A 2012 analysis by London’s Health Protection Agency that reviewed 17 studies also failed to find conclusive evidence that wearing masks prevents influenza infection.
The reasons for those results—how people wear masks, the nature of influenza, differences in cultural norms, or something else entirely—is impossible to ascertain for now. Why? “The science in support of masks keeping us from getting infected is not strong,” concludes Jared Baeten, a vice-dean at the University of Washington’s school of public health.
Studies on masks’ efficacy are extraordinarily difficult to do. Enlisting millions of people to wear masks during flu season, and comparing their infection rates to people who do not, simply hasn’t been done—nor could it, really. That’s left scientists struggling to compare observational studies from places such as Asia (where mask-wearing is prevalent) with places like the US or Europe where it is not. Drawing statistically valid comparisons is difficult, if not impossible.
Mathematical models offer one form of clarity. When just 50% of the population wears masks, say researchers simulating outbreaks, the share of the population infected by the virus is cut in half. Once 80% of the population wears a mask, it theoretically stops an outbreak in its tracks. “Any type of general mask use is likely to decrease viral exposure and infection risk on a population level, despite imperfect fit and imperfect adherence,” notes a 2008 study by the Netherland’s National Institute for Public Health and the Environment.
But all of this is highly theoretical, says Matthew Lamb, an epidemiologist at Columbia University’s Mailman School of Public Health. Since humans and viruses are messier than computer models tend to acknowledge, these findings fall apart in the real world.
“Modelers estimate that masks may help, but when studies are actually done in a general population there isn’t any real population effect,” says Lamb, an infectious disease prevention specialist. “The problem may be a lack of good studies or that the modeling assumptions are optimistic.”
Give a first opinion
That doesn’t mean public health officials must remain on the fence. The first line of defense will always be social distancing, hand-washing, sterilizing surfaces, and avoiding touching one’s face. But researchers in the medical journal The Lancet argue that (pdf) health agencies must consider asking the public to wear masks, even without strong evidence.
“It is time for governments and public health agencies to make rational recommendations on appropriate face mask use,” they wrote on March 20. “There is an essential distinction between absence of evidence and evidence of absence.” As a result, they argue it’s now “reasonable to suggest” surgical masks for all vulnerable individuals in crowded, high-risk places.
For Covid-19, this precaution is especially reasonable. Many people are contagious before they fall sick, or show any symptoms at all. Asian nations including South Korea, Taiwan, Singapore, and China have beaten back outbreaks through a combination of mass testing, contact tracing, and social distancing. Widespread use of masks in Asia, where it is considered a civic duty thanks to a century-long history of wearing masks to cope with epidemics, may cut down on viral transmissions in crowded, dense urban environments. At the peak of the 2003 SARS epidemic in Hong Kong, 76% of the population wore a face mask. In the coronavirus pandemic, surveys by Hong Kong health authorities suggest 97.5% of the general adult population wears masks when leaving the house. UPDATE Mar. 30: Germany is now considering making facemasks compulsory and Austria will make wearing them mandatory in supermarkets.
None of this comes without risks. The US could manufacture or import millions (ultimately, billions of masks) and embark on a mass education campaign. “That’s a big risk” in the West, says Baeten, if it leads to more risky behavior because people assume they’re safe and adherence is low, eliminating any benefits of wearing masks.
To really answer this question, governments need to study the question more seriously. The scientific literature is littered with small experiments and haphazard observations. Recruiting a few hundred college undergraduates for an experiment will never be enough.
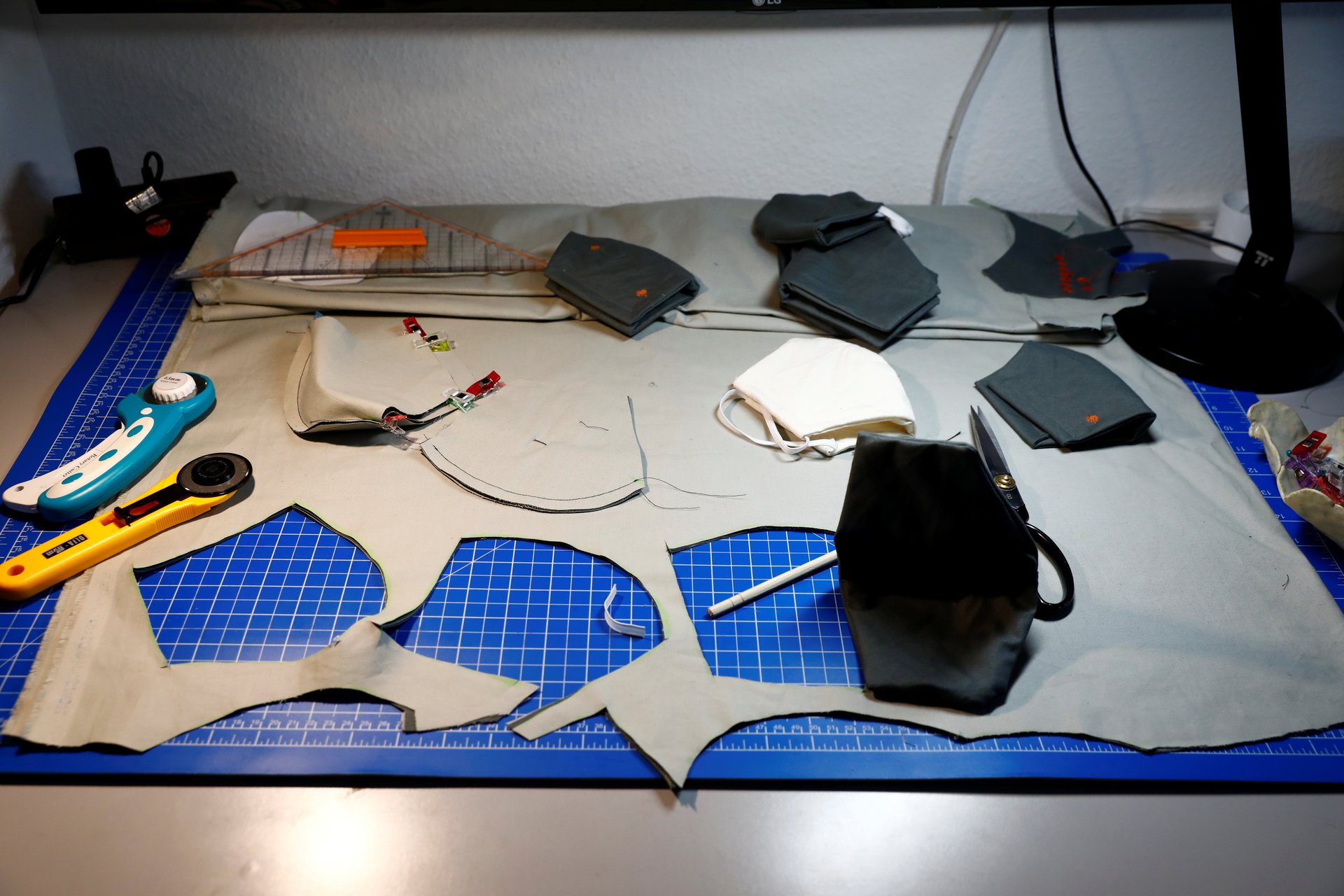
The uncertainty has left countries like the US in agonizing straits. Doctors and nurses who need masks right now are left to battle the epidemic unprotected. Masks cannot be found at any price with stockpiles exhausted and panic buying emptying warehouses. The public is left hoping the medical professional who care for them are protected, even as they try to protect themselves. Some have started donating their masks to hospitals.
Definitive answers are only possible if scientists can conduct population-trials among many thousands of people over several flu seasons. No one has ever done such a study. But doctors are learning quickly in the midst of the pandemic, and it may change our desire to answer the question once and for all.
“I don’t think we’ll have crisp answers by the end of this,” says Noymer. “I do think there will be more willingness to study it.”