Why it’s worth spending a billion dollars a year to eradicate polio
Tomorrow, the World Health Organization (WHO) is expected to officially certify that south-east Asia, formerly one of the regions with the worst levels of polio, has eradicated the disease, after India found new no cases in the previous three years. (The WHO counts India as part of south-east Asia.) To understand why that matters, read this heart-breaking profile of Rukhsar Khatoon, the four-year-old girl with India’s final documented case of polio.


Tomorrow, the World Health Organization (WHO) is expected to officially certify that south-east Asia, formerly one of the regions with the worst levels of polio, has eradicated the disease, after India found new no cases in the previous three years. (The WHO counts India as part of south-east Asia.) To understand why that matters, read this heart-breaking profile of Rukhsar Khatoon, the four-year-old girl with India’s final documented case of polio.
The news comes at a key time for the people trying to stop polio for good: They’ve missed their deadline several times and need a global push to make polio the second human disease, after smallpox, to be eradicated outright.
The Global Polio Eradication Initiative (GPEI) originally hoped to rid the world of polio by 2000, but eliminating the final cases has proven much harder and more expensive than its advocates had hoped. The cost has stretched past $10 billion, much of it fronted by donors from wealthy countries that have already eliminated the disease, as the US did in 1979. For comparison, eliminating smallpox cost $500 million in 2008 dollars.
Some public health advocates have questioned whether all this expense really is worth it or if eradicating the disease is even possible. They argue that the money saved by merely managing polio, rather than eliminating it, could be better used fighting other diseases, like AIDS or malaria, that ravage developing nations. Nonetheless, last year the GPEI announced plans to spend an additional $7 billion to eliminate the disease by 2018.
The GPEI’s case is that, while trying to eradicate polio is more expensive up front, trying to merely keep it under control will be more expensive in the long run. Polio affects mainly children and in one in 200 cases, it leads to irreversible paralysis that requires life-long care. Eradicating polio in the US is estimated to have saved some $220 billion since 1955. An economic analysis (pdf) by infectious-disease experts estimated that by preventing some 8 million cases of polio paralysis from 1985 to 2035, the GPEI will create net gains of $40 to $50 billion, mostly in the developing economies.
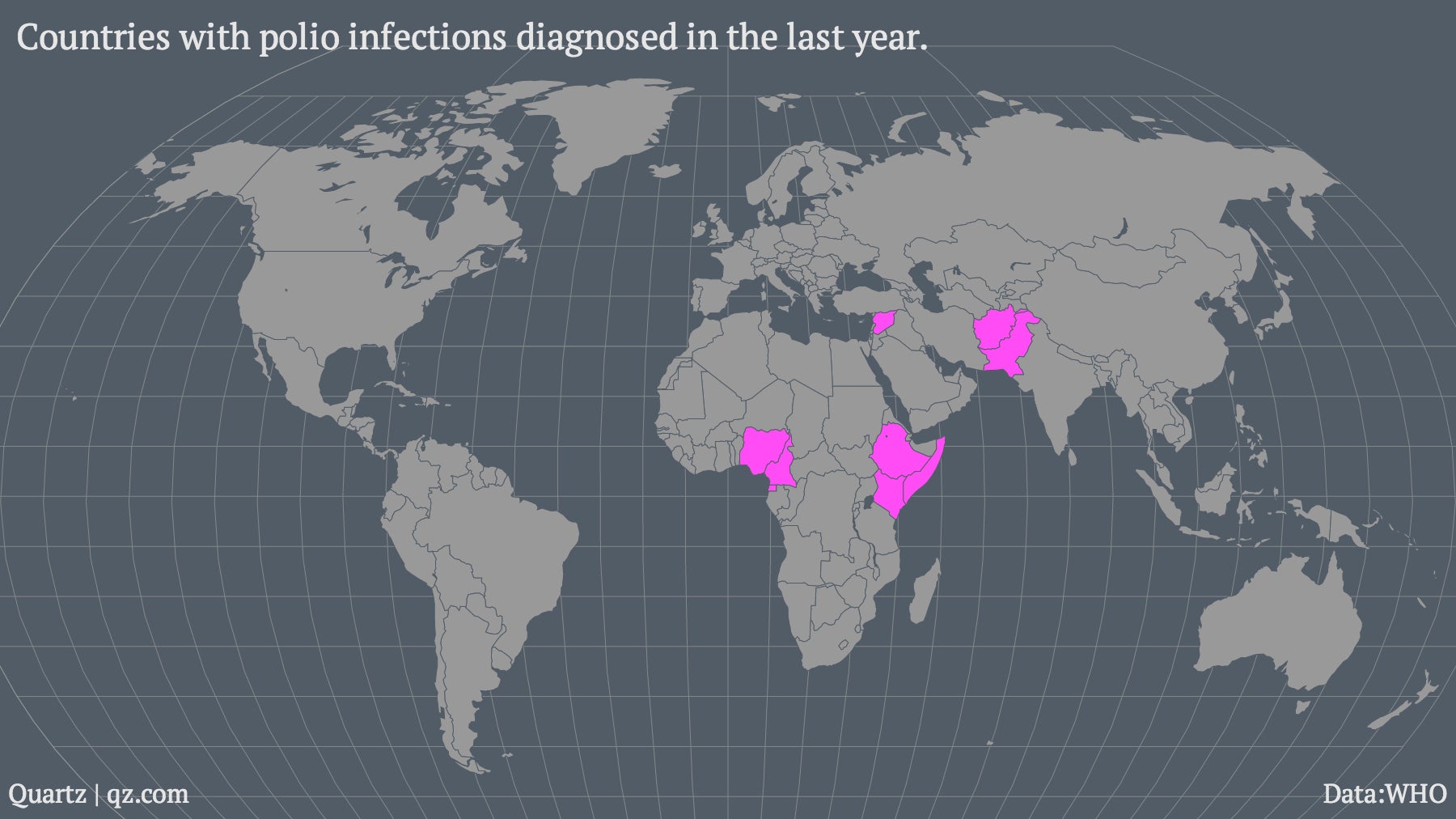
Also, if polio is controlled but not eradicated, it’s expensive to respond to outbreaks when they happen. After certain states in Nigeria briefly stopped delivering vaccines in 2003, GPEI says it spent $220 million dealing with the resultant outbreak. Last year also saw the first reported polio case in Equatorial Guinea since 1999, when a virus from Cameroon exploited a drop in the routine vaccination of children. That’s why eradication advocates are reluctant to rely on existing vaccination infrastructure as a way of controlling the virus.
Their fear is that pulling back resources from eradicating polio to focus on other health problems will create a permanent pool of polio victims, and any money not spent on eradication will soon be eaten up by the costs of care and outbreaks. This chart from GPEI (pdf) compares the cost of three eradication scenarios—from most to least comprehensive—plus two control scenarios that involve continuing to immunize people without trying to wipe out the disease.

Still, these analyses have been made before, and turned out to be premature. In 1998, researchers forecast that the eradication of measles in the US by 2010 would save $45 million a year. Despite official “eradication” in 2000, cases of the measles are growing again thanks to the anti-vaccine movement’s push against immunization. That’s why the victory in India is so important for public-health advocates—it shows that even in a country with far weaker medical facilities and a lot more ignorance than the US, a concerted effort can still wipe out a disease.