The US could have 50 million vaccine doses before it’s ready to use them
The US Food and Drug Administration (FDA) may not authorize a Covid-19 vaccine until January 2021 at the earliest, according to Anthony Fauci, director of the US National Institute of Allergy and Infectious Diseases—but that isn’t stopping drug manufactures from cranking them out by the millions ahead of time.
The US Food and Drug Administration (FDA) may not authorize a Covid-19 vaccine until January 2021 at the earliest, according to Anthony Fauci, director of the US National Institute of Allergy and Infectious Diseases—but that isn’t stopping drug manufactures from cranking them out by the millions ahead of time.
Between Moderna and Pfizer, makers of the two vaccines emphasized in federal distribution preparedness plans, the US should have access to at least 50 million vaccine doses by the end of 2020. Assuming each person receives two doses for maximum immunity, that’s enough to vaccinate 25 million Americans—less than 10% of the US population. But until the FDA gives the green light, those doses will have to stay in cold storage.
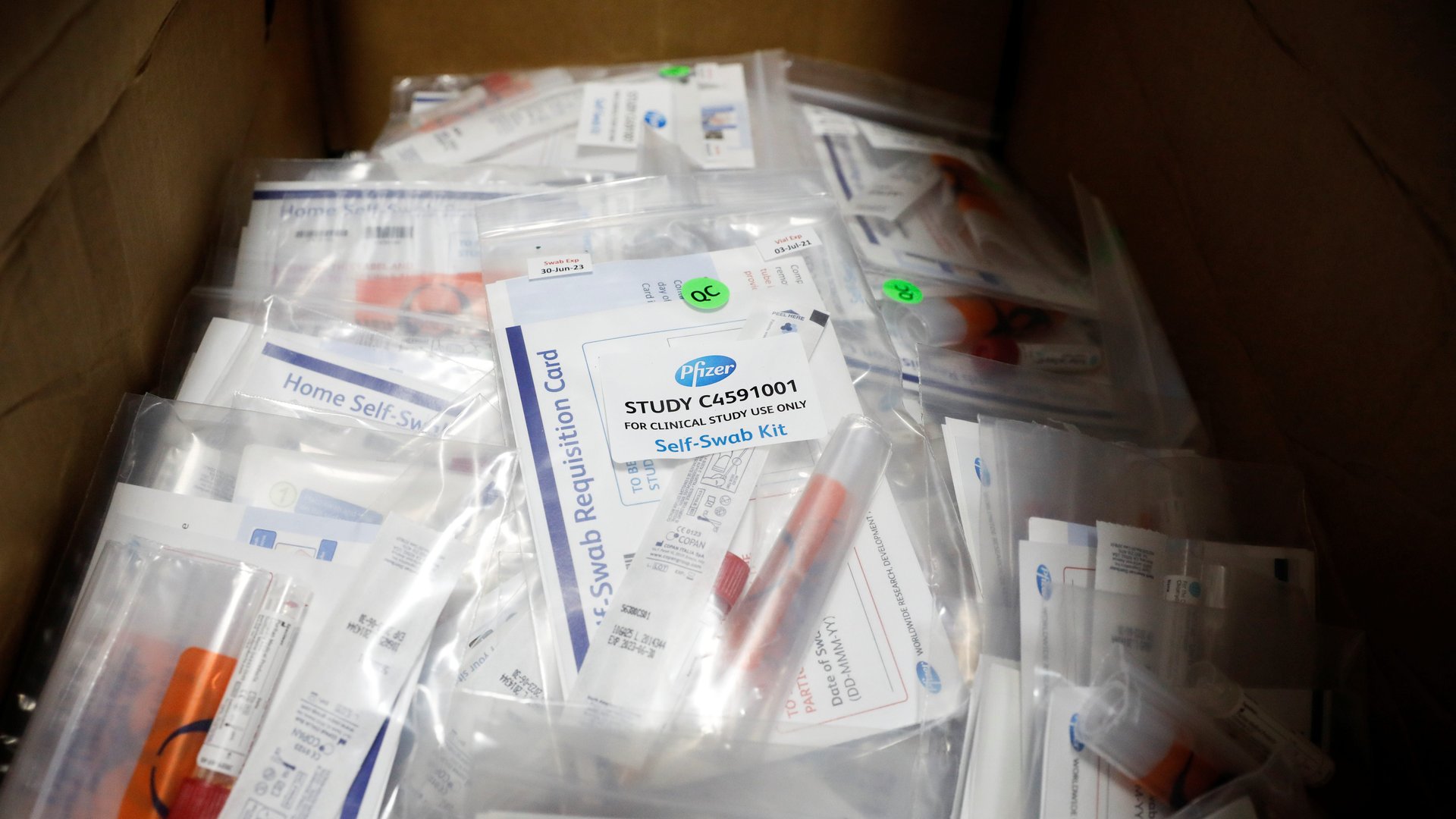
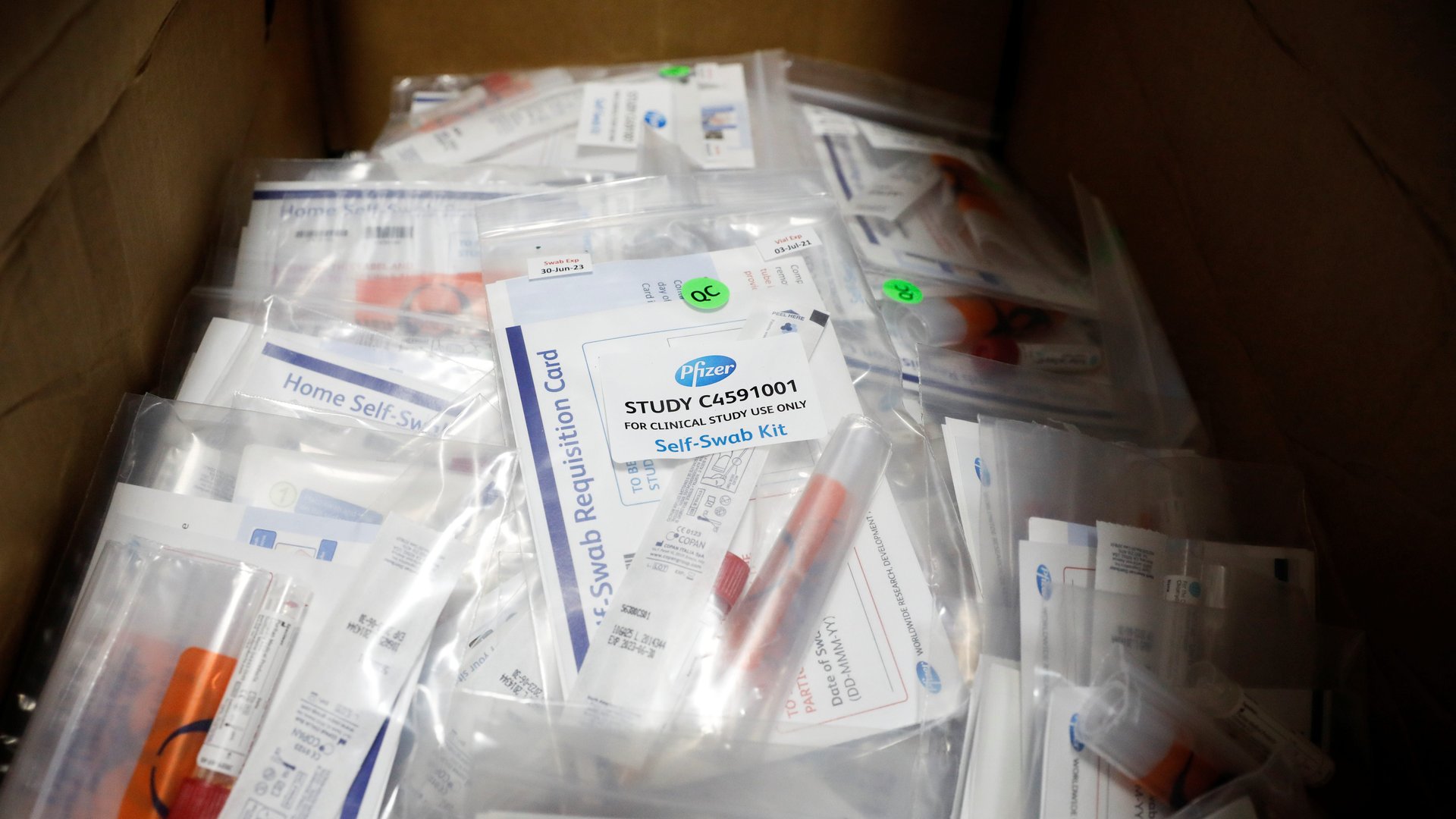
In an earnings call on Oct. 23, Pfizer CEO Albert Bourla stated that the company had already made “hundreds of thousands” of doses of its Covid-19 vaccine candidate; he expects to have 30 million to 40 million doses ready to deliver to the US by the end of the year, with plans to reach 100 million by March 2021. And today, Oct. 29, Tal Zaks, the chief medical officer of Moderna, said that he expects to be able to provide 20 million doses of its candidate to the US by the end of the year.
The US government has invested in both companies to ensure speedy access to their products if proved safe and effective. It provided nearly $2 billion to Pfizer through Operation Warp Speed, and nearly $1 billion to Moderna through multiple investments through the Biomedical Advanced Research and Development Authority. Both companies are wrapping up their late-stage clinical trials, but have yet to share the data examining their vaccines’ safety and efficacy profiles.
The US has spread out its vaccine bets: It also invested in Johnson & Johnson, AstraZeneca, and Novovax, which are also ramping up vaccine manufacturing. But Pfizer and Moderna have made the most progress in their phase 3 trials. Novovax’s phase 3 trial has been delayed until next month, and both Johnson & Johnson and AstraZeneca just got clearance to resume their phase 3 trials last week after they paused to investigate potentially dangerous adverse reactions.
Manufacturing so many vaccines before approval isn’t arrogance—it’s by design. Drug manufacturers are antsy about the manufacturing bottleneck that could occur as soon as a vaccine gets the all clear. Each of the vaccines in the pipeline require their own factory setups and equipment. Space and gear are finite resources; even after a candidate clears the hurdle of a phase 3 clinical trial, it could take months for these factories to catch up with demand. The US’s Operation Warp Speed initiative bought first dibs on 300 million doses of potential Covid-19 vaccines in anticipation of this bottleneck.
What’s not yet clear is who will be first in line to get these doses once they’re available—which should be within 24 hours of getting the green light from the FDA. Those who work in healthcare and have the highest risk of exposure are likely to be first in line. After that, cities and states are likely to prioritize the elderly and immunocompromised, who are at the greatest risk of developing severe complications from Covid-19, but their vaccine deployment plans are still under review by the federal government.