Vaccines won’t eradicate Covid-19—and that’s ok
Countries that never got the pandemic under control—like the US, the UK, and Brazil—have waited patiently for a Covid-19 vaccine. Now that they’re finally trickling out into the waiting arms of the public, it’s still not enough to go back to normal.
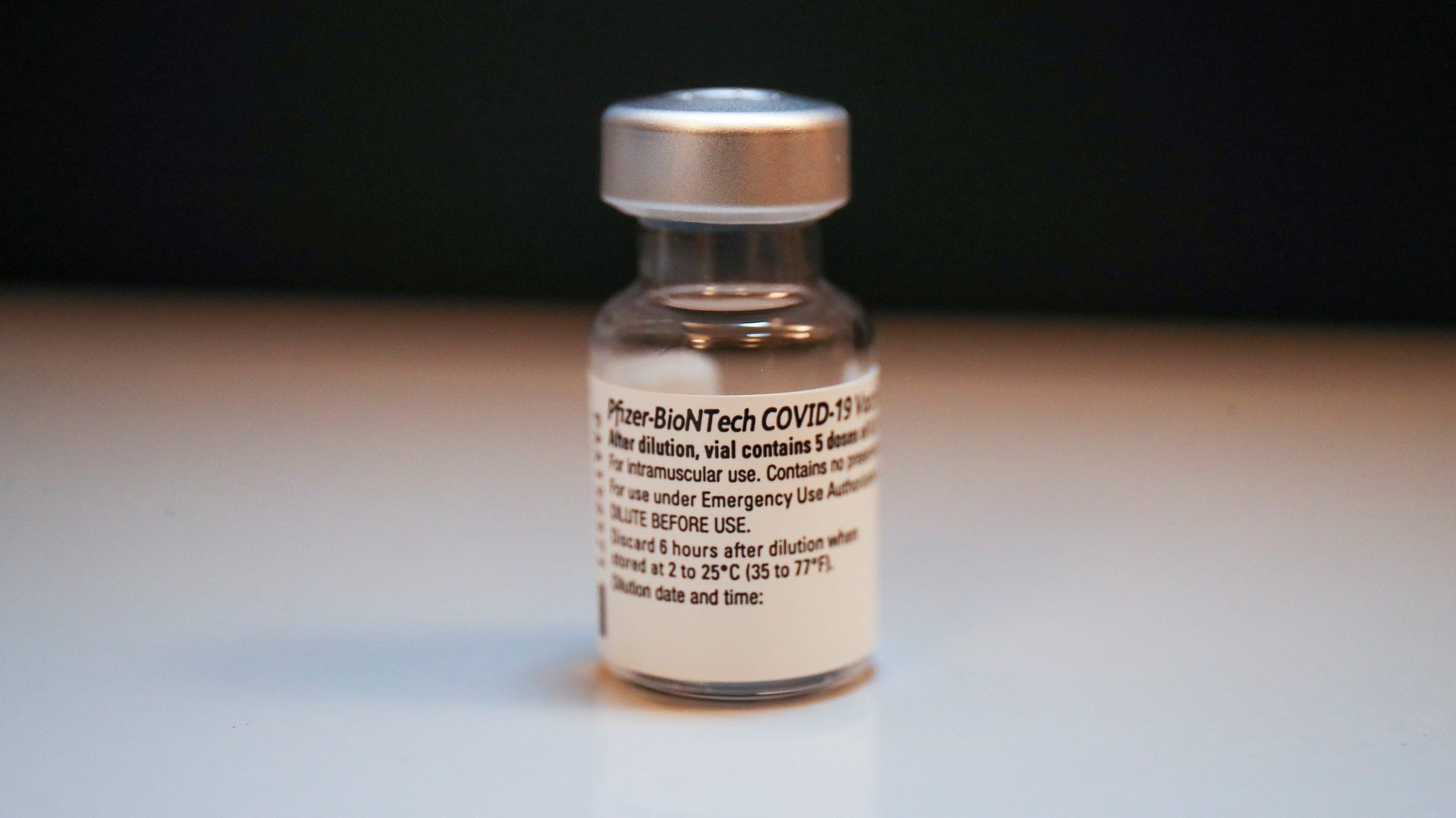
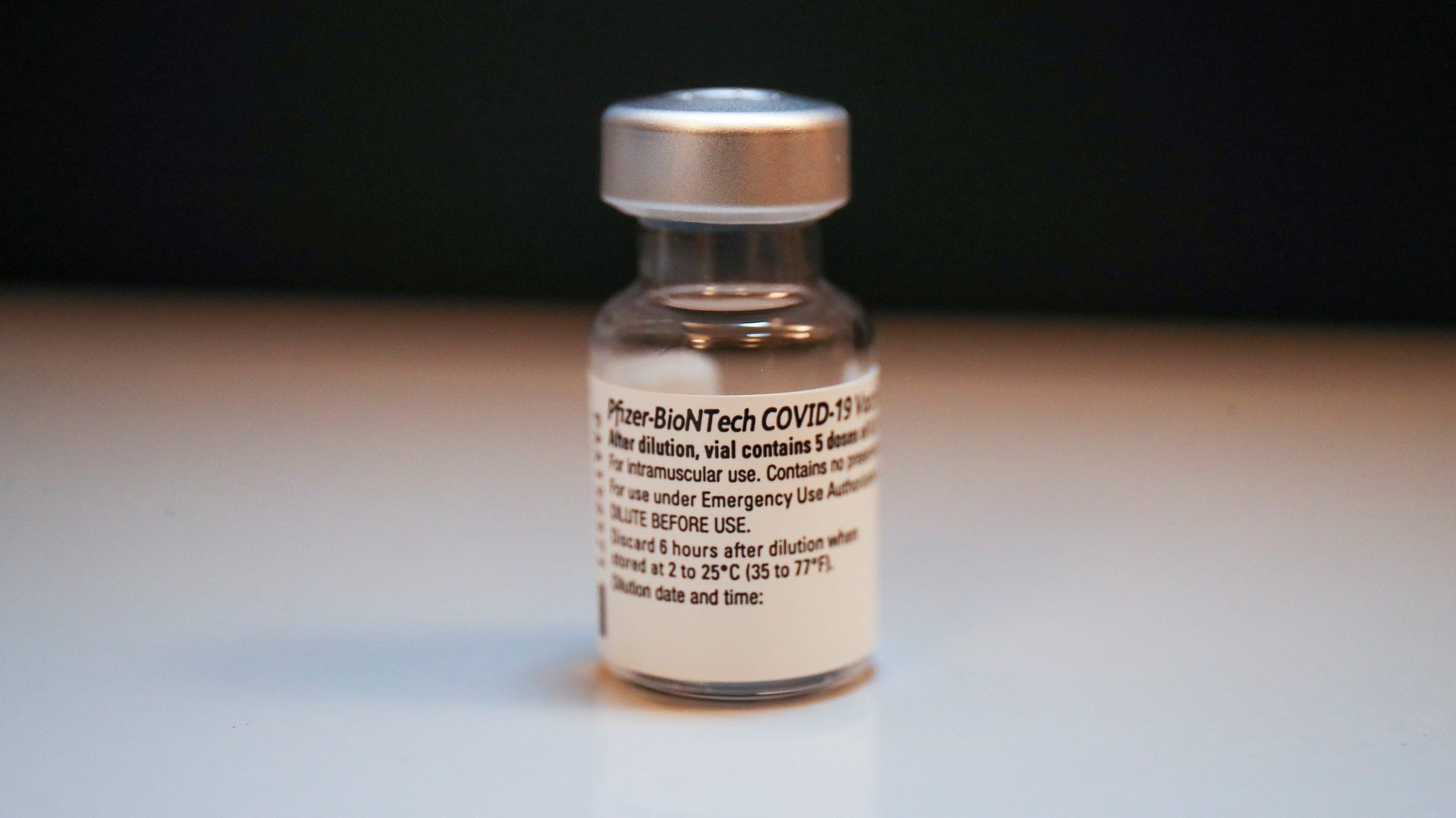
Countries that never got the pandemic under control—like the US, the UK, and Brazil—have waited patiently for a Covid-19 vaccine. Now that they’re finally trickling out into the waiting arms of the public, it’s still not enough to go back to normal.
There are a lot of reasons for these delays. Some are related to ongoing research: Scientists are still investigating how well available vaccines protect against new variants of the SARS-CoV-2 virus, and how well they prevent transmission. Others fall outside the realm of science, like manufacturing bottlenecks, distribution challenges, vaccine hesitancy, and fear of medical establishments spreads through social media.
Regardless of the reasons why the Covid-19 vaccines haven’t brought us to a new normal, “pandemic fatigue” has set in. Despite the speed with which these vaccines were developed, roadblocks and uncertainties—and the precautions they necessitate—are leading to disillusionment with vaccines in general.
It’s easy to let this exasperation undermine our optimism that the pandemic will ever end. But only talking about the problems vaccines can’t or haven’t yet solved makes us forget that vaccines are vital public health power tools. And although all tools need to be used effectively to get a job done, they’re still worth celebrating.
Invisible infrastructure
The most successful vaccination effort to date eliminated the pathogen it protected us from.
In 1980, the World Health Organization declared that smallpox was officially eradicated. That disease, also caused by a virus, killed one-third of the people it infected, and left others blind or with disfiguring scars.
It didn’t happen overnight. Edward Jenner concocted the smallpox vaccine, the first against a pathogen, (with incredibly questionable study methods) in 1796. It was the first vaccine against an infectious disease. And yet, it would take almost 200 years to vaccinate enough people to stop the spread of the disease entirely.
More recently, the polio vaccine has nearly eradicated the virus. A handful of outbreaks still exist in Pakistan, Nigeria, and Afghanistan where violence and political instability have kept healthcare providers from delivering vaccines.
Though these vaccinations are success stories, they’re partly a product of circumstance. Polio largely affects children, which means it’s logistically easier to ensure they receive their shots. In many jurisdictions, schools require children to receive the polio vaccine (among others) which serves as something of a checkpoint that entire generations have to pass through. And though Jenner’s smallpox vaccine came before modern medicine (and manufacturing), it was easier to quarantine incoming ships or sick patients, so the virus spread more slowly
But with SARS-CoV-2, the virus that causes Covid-19, “we’ve set ourselves a bigger challenge than we had in the past,” says Amy Bix, a medical historian at the University of Iowa.
For one thing, the virus targets people of all ages. Adults don’t have the universal vaccination requirements like students. The only requirements for adult vaccinations today are for international travel, and even those are rare. For another, SARS-CoV-2 has unprecedented opportunities to spread. Globalization and advances in travel give infections the opportunity to jump from country to country in a matter of hours instead of days or weeks.
Of course, there are tremendous benefits to living in a modern, global society. Other medical advancements—including other vaccines—have raised life expectancies globally. We don’t even know how many cases of measles or mumps vaccines have been prevented because it’s impossible to prove, says Bix. And technological feats enable near instant communication with friends across the world. For the most part, we’re used to living free from fear of dying young, and having quick solutions to any problem at our fingertips.
History is full of examples of progress benefiting only a select group of people, but vaccines, for the most part, stand out for having benefited the majority of people on the planet. We just don’t see them that way because we’re so accustomed to life with their protection.
The problems Covid-19 vaccines can’t solve
In terms of Covid-19 vaccines, plenty of progress remains to be made. Some of it just takes time. Despite developing and administering vaccines against Covid-19 within a year of discovering the virus, pharmaceutical companies are still studying if different kinds Covid-19 vaccines can be mixed, how long they’ll offer immune protection, and to what degree they stop transmission. “The thing about medical research is there are some parts you can hurry and there are some parts you literally can’t,” says Bix.
There’s also the issue of vaccine inequalities that need to be addressed, too. “Prioritization plans have taken racial equity into account, but only nominally,” Julia Marcus, an epidemiologist at Harvard University, wrote in The Atlantic. The groups most likely to develop Covid-19 are the ones least likely to get vaccines. They’re also most likely to suffer disproportionate economic hardships, something the pandemic has exacerbated.
Knowing that vaccines can’t solve all the problems caused by the pandemic, we have to look elsewhere. “We have to think, ‘How could we make life better for people who had things worse?’” Bix says. This is where community leaders and politics come in: They can shape how to educate and prioritize vaccine recipients, or control the funding that could alleviate some of the other pandemic-induced hardships.
In all of modern medicine, vaccines have served as tools. They’ve never been a complete fix, and certainly can’t be a solution to a pandemic of Covid-19’s magnitude. But by focusing only on the uncertainties around them, or how they’ve failed to reopen society yet, we lose sight of how powerful they actually are: Slowly but surely, fewer people will get sick, and fewer will be hospitalized. Severe cases will be reduced to mild. And eventually, we will reach a new normal where restaurants, travel, and parties will once again be safe.