A ‘just-add-water’ kit to make instant drugs and vaccines could fix health care access in rural areas
Soon, getting medical assistance to rural areas—where half of the world’s population still lives—won’t be hindered by power outages anymore.


Soon, getting medical assistance to rural areas—where half of the world’s population still lives—won’t be hindered by power outages anymore.
In developing countries (where the majority of the world’s rural residents live), infrastructure is weak, there is a dearth of qualified medical personnel, and resources like electricity are low or sporadically available. As a result, medical supplies often don’t reach remote areas, or if they do, there’s often no functioning refrigerator to store them in. One solution would be to find a cheap way to produce those supplies on the spot.
A team of researchers at University of Toronto and Harvard University’s Wyss Institute for Biologically Inspired Engineering are working on just that. They are pioneering a technology that could allow people with minimal training to produce a broad range of medication, including diagnostic tools, vaccines, and drugs, anywhere in the world.
The process draws on prior research by the team, where they discovered that DNA translation and transcription can work outside of a living cell. Then, they embedded that synthetic genetic information into inexpensive materials like paper, making possible in-vitro applications in the clinic and out in the field. The team first developed a paper-based tool to identify the Ebola virus in 2014, then adapted the technology in May 2016 to detect the Zika virus. For each disease, the researchers embedded programmable synthetic gene networks on paper, which acts almost like a litmus test, changing color when the strain of virus is detected.
“Stable at room temperature, these paper-based synthetic gene networks are readily stored and distributed, and are activated by simply adding water or a biological fluid sample,” the researchers explained in their 2014 paper. At this point, these demos are proof-of-concept and human testing does not have a set start date yet.
Now, the team is advancing the technology from diagnostics to treatment, employing two types of freeze-dried pellets: One has the cell-free “machinery” to synthesize the end product—a drug or vaccine. The other contains DNA instructions that will tell the “machinery” what compound to manufacture. Much like stirring water to store-bought freeze-dried yeast and sugar will activate the yeast and make the bread rise, adding water to both pellets kickstarts the biochemical processes that manufacture desired products. When the pellets are rehydrated, the DNA encodes the intended protein within one or two hours.
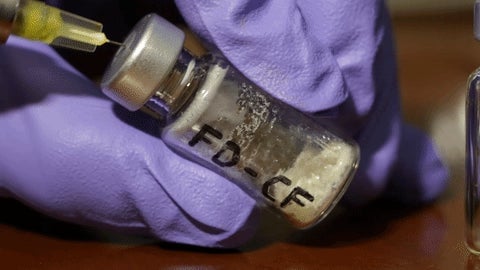
A variety of uses are outlined in a recent paper published in Cell: routinely manufacturing batches of tetanus or flu shots in remote clinics, quickly mobilizing vaccines against emerging infectious disease outbreaks to prevent epidemics, and more. So far, the researchers have demonstrated over 54 portable manufacturing uses and validated them through cell-based and in-vitro tests outside the body or animal trials.
In one instance, at least 33 human doses of diphtheria vaccine were generated using a 900 milliliter pool of pellets and mice tests delivered promising results. “We were able to induce the specific antibody response in the mice and they were healthy,” says University of Toronto assistant professor Keith Pardee, the lead author on the paper.
In the diphtheria example, the researchers were able to keeps costs at $10-$18 per dose—close to the $16.73 Center for Disease Control contract price for a dose of DTAP (diphtheria, tetanus, and pertussis) vaccine. However, those costs could drop. “Right now, it’s going to be the most expensive time for these products,” Pardee said. “As we become better at developing these tools and the community keeps improving the yield, the cost will continue to fall.” Plus, there’s huge cost savings in transport and storage— ready-to-use vaccines have to be refrigerated at all times, but these kits can be stored at room temperature and manufactured on an at-need basis.

Freeze-dried cell-free biomanufacturing platforms could eliminate “the need for a cold supply chain,” says Northwestern professor Michael Jewett, who is not associated with the research but specializes in synthetic biology. “By moving manufacturing from the factory to the front lines, we might be able to provide patient-specific medicines where medicines are not available now.” The technology could not only provide better access to costly drugs through decentralized production in rural areas with power shortages, but one day, astronauts could even carry it into space