Stem-cell therapy is poised to disrupt the Tommy John epidemic in baseball
For about half a decade, it’s been something of an open secret in baseball that players—pitchers especially—regularly undergo stem-cell therapy to stave off surgeries and lost playing time. It’s a cutting-edge medical procedure, done by everyone from high-school standouts to major-league all-stars. It’s rarely discussed by players, or by their coaches, parents, doctors, or employers.


For about half a decade, it’s been something of an open secret in baseball that players—pitchers especially—regularly undergo stem-cell therapy to stave off surgeries and lost playing time. It’s a cutting-edge medical procedure, done by everyone from high-school standouts to major-league all-stars. It’s rarely discussed by players, or by their coaches, parents, doctors, or employers.
So when the Los Angeles Angels went public in 2016 with the news that first Andrew Heaney and then Garrett Richards were undergoing stem-cell therapy for torn ulnar collateral ligaments (UCLs), it was both anticlimactic and a revelation. For the first time, baseball pitchers and their employers were openly admitting trying this novel procedure that, while fairly well-proven anecdotally, has yet to be validated by any well-designed scientific study.
By now, that so-called Tommy John surgery for a torn or damaged UCL has become a rite of passage for the top-flight professional baseball pitcher is a cliche of sports punditry. Every young arm that can fold and then unfold itself into tortuous patterns that facilitate throwing baseballs at 95 miles per hour or faster is bound for the knife, once those upper body contortions inevitably tear the tissue on the inside of their elbows connecting their upper and lower arms, the UCL.
The first Tommy John surgery (or more properly, UCL reconstruction) was performed in 1974 by the orthopedic surgeon Frank Jobe, then the team physician for the Los Angeles Dodgers, on the eponymous pitcher. It was a great success; Tommy John came back to pitch 14 more years in the pros, racking up 164 wins with four different teams.
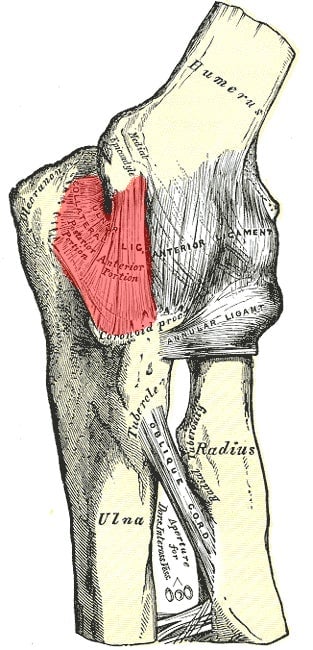
TJ surgery is fairly straightforward: the connective tissue that makes up the UCL is either replaced with a tendon taken from elsewhere in the patient’s own body or from the donated tissue of a cadaver.
Nevertheless through the mid-1970s and into the ‘80s, TJ was something of a rarity; just a handful of baseball players underwent that particular knife. In the 1990s the numbers started to tick up, and then in the 2000s, they exploded. From 1995 to 2005, there was an average of 28 TJ surgeries per year across all levels of pro baseball; from 2005 to 2015, there was an average of 84 TJ surgeries per year.
Then something strange happened. In 2016, the total number of TJ surgeries performed dropped to 90, from 127 the year before, a 30% decline. Only one other year in Tommy John history, 2008, saw such a precipitous drop from the previous year. By 2009, TJ numbers were back to 2007 levels; obviously it remains to be seen whether 2017 will look more like 2015 or more like last year. But the data suggest that if TJ surgery numbers are in fact starting to trend downward, it might have something to do with the rise of stem-cell therapy.
What makes stem cells unique is that they are what’s called “undifferentiated”; they can become other specialized cells depending on the body’s need at the time. There are two types of human stem cells, embryonic and adult. Embryonic stem cells come from a very early-stage embryo; these are what you likely think of when you hear the term “stem cells”—they’re at the center of one of most exciting fields of medical science research today. Embryonic stem cells are now used or are being studied for a shockingly wide range of applications, from Alzheimer’s and autism to vision impairment and infertility. However, thanks to the religious right-driven opposition to the harvesting, study, and use of embryonic stem cells, they’ve been mired in controversy in the US.
On the other hand, the use of “adult” stem cells—which can be harvested from bone marrow, fat, or blood of any person of any age (the name is a bit misleading)—is widely accepted by both the medical community and politicians. They have less range, so to speak, than embryonic stem cells; they are primarily to repair and replace damaged tissue in the area they are found. That makes them just about perfect for repairing a torn UCL.
The first pro baseball player known to have undergone stem-cell therapy for a UCL weakness was Bartolo Colon—and he was basically forced into talking about it. Following a long run of success culminating with a Cy Young Award season in 2005, Colon had four frustrating years racked with injury and ended up unsigned after 2009. He took a year off to recuperate and in spring of 2011, he was back, signed with the New York Yankees and feeling good. Serge Kovaleski, an investigative reporter with the New York Times, started digging into how Colon had made his comeback, and uncovered the name of Joseph Purita, an orthopedic surgeon and stem-cell therapy pioneer.
As Purita tells it, there was nothing illegal or nefarious about the work he’d done on Colon; there was just never a plan to broadcast it, either. Then, he recalls, “the Times called me up and said ‘we’re going to write a story whether or not.” So, Purita offered details. In April 2010, he told the paper, a team of Dominican doctors used stem-cell therapy to help repair Colon’s ligament damage and torn rotator cuff.
Colon’s recovery was a resounding success. He’s been an all-star twice, is the current active leader in major league wins, and, at age 44, is signed to a $12.5 million contract to be the Atlanta Braves’ number two starter for the 2017 season.
But instead of thrusting stem-cell therapy into the mainstream, the Colon incident forced it to stay underground. The treatment was not well understood at that point, and the circumstances—that it was done offshore, that it was unearthed by investigative reporting, and that, in 2012, Colon was suspended for 50 games for testing positive for testosterone use—clouded public opinion on it. Many were convinced Colon had gotten performance-enhancing drugs in the Dominican Republic. Purita denies this vociferously, and MLB inquiries back him up.
The upshot is that every doctor I spoke to who studies and performs stem-cell therapy for torn-ligament repair says some version of the same thing: “I can’t give names but there are some professionals” who have come in for treatment, says Joshua Dines, an orthopedic surgeon at New York’s Hospital for Special Surgery, and an assistant team physician for the New York Mets.
Purita says that since Colon, he’s worked with some players that “had team approval—and some just come on their own,” but none wanted to go public about the procedure.
If use of your arm is mostly limited to spreadsheet jockeying and lifting forkfuls of pasta or salad from plate to maw, TJ is no big deal—in that case, you’re ready to go back to work in six weeks. But if you throw a ball at top speed past another pro athlete for a living, you’re going to be out of commission for 18 months or more as you regain strength in your money arm.
And money is the (post) operative word. In 2016 alone, MLB teams lost nearly $60 million in player value because they had to fulfill dozens of contracts of players recovering from Tommy John. That’s nearly enough to field an entire pro team—definitely enough to roster a top-of-league pitching staff. And that $60 million doesn’t come close to accounting for the losses suffered by players who had to undergo the knife during the last year of a contract, and found themselves released by their previous teams with no new offers on the table while they recovered.
There was never going to be a way to prevent the need for Tommy John surgeries. Baseball players throw far too hard, with far more breaking pitches, starting at far too young an age, to realistically stop UCLs from tearing (though all sports medicine experts do now warn coaches and parents to keep kids and teens at low pitch counts). The alternative was always going to be something that could cure ligament tears—but better than TJ surgery, with a faster recovery time.
Everything we’ve seen in the past decade or so suggests stem-cell therapy is exactly that. At this point, platelet-rich plasma (PRP) injections are common first-line defenses against UCL injuries. The procedure entails harvesting PRP from the player and injecting it into the injured part of the body. PRP is dense with proteins specialized for injury repair.
You can think of these injections as a precursor to stem-cell therapy; both are considered “biologic” treatments and entail wielding the body’s own weapons against injury. Many of the doctors now doing stem-cell therapy started off with PRP procedures. When baseball players have a torn ligament, they typically try PRP first. If that fails, it’s Tommy John time.
Except, everyone in the field says that at this point PRP is last decade’s technology, more than ready to be replaced by stem-cell therapy, which does much the same thing but better. Adult stem cells essentially are there for the very purpose of tissue repair. Why not take them from a part of the body that’s all good, and send them to a region where reinforcements are desperately needed?
Dines says that in his own practice, he’s been able to cut down the need for Tommy John surgery by about a third, thanks to his reliance on stem-cell therapy. He doesn’t believe that the procedure will lower the number of players that have to have TJ, but it will limit the number of overall TJ surgeries—because at this point, many pitchers have to get the surgery twice in their career. Dines says stem-cell therapy can get 15- or 16-year-old pitchers through their first partial tear. They may still need to get a full TJ surgery by age 24, but avoiding that first one is still a “huge victory.” (A growing number of “middle-age” first-time TJ patients could also explain the overall drop in Tommy John surgeries.)
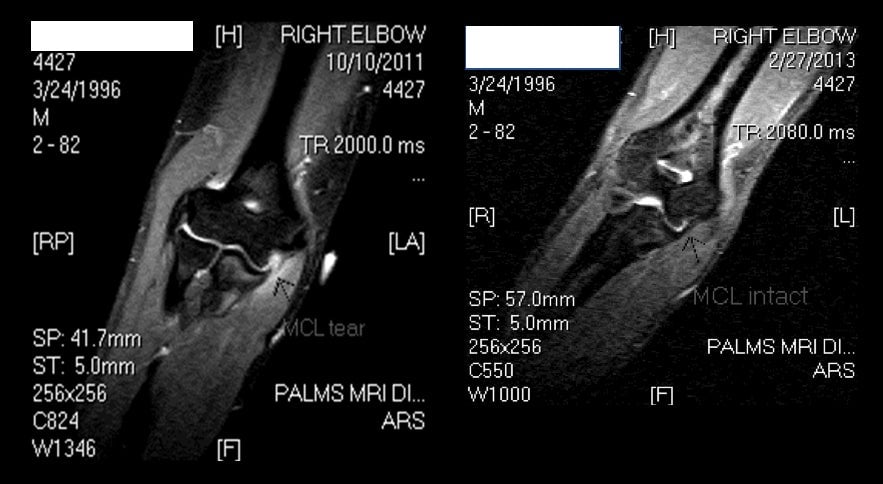
Purita is even more optimistic. While most orthopedic surgeons say that, right now, stem-cell therapy is effective on partial, but not full, ligament tears, Purita is confident his version can handle any UCL. He sent Quartz a photo showing a patient—an MLB pitcher who wishes to remain anonymous, Purita says—who had a full UCL tear in November 2011 and, after receiving stem-cell therapy at Purita’s clinic, made a full recovery by February 2013.
“You never say something replaces something else entirely,” Purita says. “Stem-cell therapy is not going to replace every case [of Tommy John], but it could probably replace the majority of cases.”
Talk to anyone who knows the field and they’ll rattle off the same reasons why stem-cell therapy for UCL tears isn’t already the standard of care: One reason is that, relative to the population, the number of UCL tear patients is extremely small, which means there’s only a tiny pool from which to draw potential study participants. Two, a trial for a new medical treatment is typically only considered “well-designed” if the subjects are “blind”—that is, they don’t know if they are getting the real treatment or a placebo. But what kind of team or player is going to risk a million-dollar arm on a properly designed study where there’s a 50% chance that the injury gets a placebo?
That’s not to say that this is some sort of back-alley procedure. It’s performed by some of the most prestigious orthopedic surgeons and medical research centers in the US, and the US Food and Drug Administration approves its use: US doctors are allowed to harvest a person’s stem cells and use those cells to treat that same person, as long as you don’t “manipulate” (e.g. genetically modify) the cells.
The lack of literature on the procedure hasn’t exactly inspired the confidence of players and teams to go public with their decision to pursue it; nor does the fact that the procedure for years had, as Dines puts it, “a bad rap…[it] would get lumped in with things that were illegal. There was this specter of cheating.” But Dines, and others, say that’s changing.
“The needle is moving towards this being a valid way of treating things,” says Purita. People are starting to recognize that “someone making [or risking] $20 million a year is not going to do something he hasn’t checked out well.”

Amadeus Mason, a sports medicine and biologics expert at Emory University, compares stem-cell therapy today to Tommy John in the 1980s. “It was, ‘Okay, we’re going to try this and see,’” says Mason, who trained with orthopedic surgeon James Andrews. (Andrews is the Michael Jordan of ligament repair—he’s saved the arms and careers of some of the greatest pitchers in major league baseball history.) “There wasn’t a big fanfare going in” when players started with Tommy John surgeries, Mason says, “but when players came back to pitch [there] was. Same thing here.”
Mason thinks stem-cell therapy hasn’t quite reached the inflection point, but it is near. Here, too, he sees a comparison with Tommy John: “It took a while for them to perfect the procedure so that more and more doctors could do the surgery and reproduce the results well.”
Right now, Mason says, there is a relatively small handful of doctors who can do stem-cell therapy for UCL tears, but that list is growing rapidly. For example, the annual conference of the Orthobiologic Institute—a professional organization for regenerative medicine researchers and practitioners—started in 2009 with 20 or so doctors; last year’s event had nearly 1,000.
The Angels didn’t want to talk to me about why they decided to go public with Heaney and Richards’ stem-cell therapies. Perhaps that’s because Heaney’s, on May 2, 2016, was unsuccessful. The 25-year-old former first-round draft pick underwent Tommy John surgery in July of that year after failing to regain strength in his left arm. He’ll miss the entire 2017 season, setting back a promising young career.
Richards had his stem-cell procedure just 14 days after Heaney. So far, it seems to have worked. He didn’t return to pitch in 2016, but in spring training this year, he was throwing nearly 100 miles per hour. Probably the Angels’ best starting pitcher, Richards will take the mound on April 5, and all eyes will be on his right throwing arm—and on his face, to see if it is registering any pain.
If Richards stays healthy this year—and next year, and the year after that—he could become something like the 21st-century Tommy John. Every team will have a stem-cell therapy expert on its medical staff, or at least one on speed dial. Careers will be saved, and so will millions of dollars.
But wider use of stem-cell therapy also will force the MLB to confront an interesting potential side effect of the procedure. “Some players can throw faster after they have the surgery,” says Purita. “By definition, it’s making the performance better.” Right now, major league baseball does not include stem-cell therapy in its list of banned performance enhancers (pdf). But what happens when a baseball player, perhaps a fringe pitching prospect in the low minors, feels some elbow pain one day and gets an MRI, and is diagnosed with nothing—but decides to get stem-cell therapy anyway, since it could give him an extra four miles per hour on his fastball?
The MLB will have a decision to make: To accept potential competitive imbalances to save young arms, or to seek to preserve a level playing field (or even just the fiction of one) at the cost of some of the game’s best players. The question is all but inevitable.