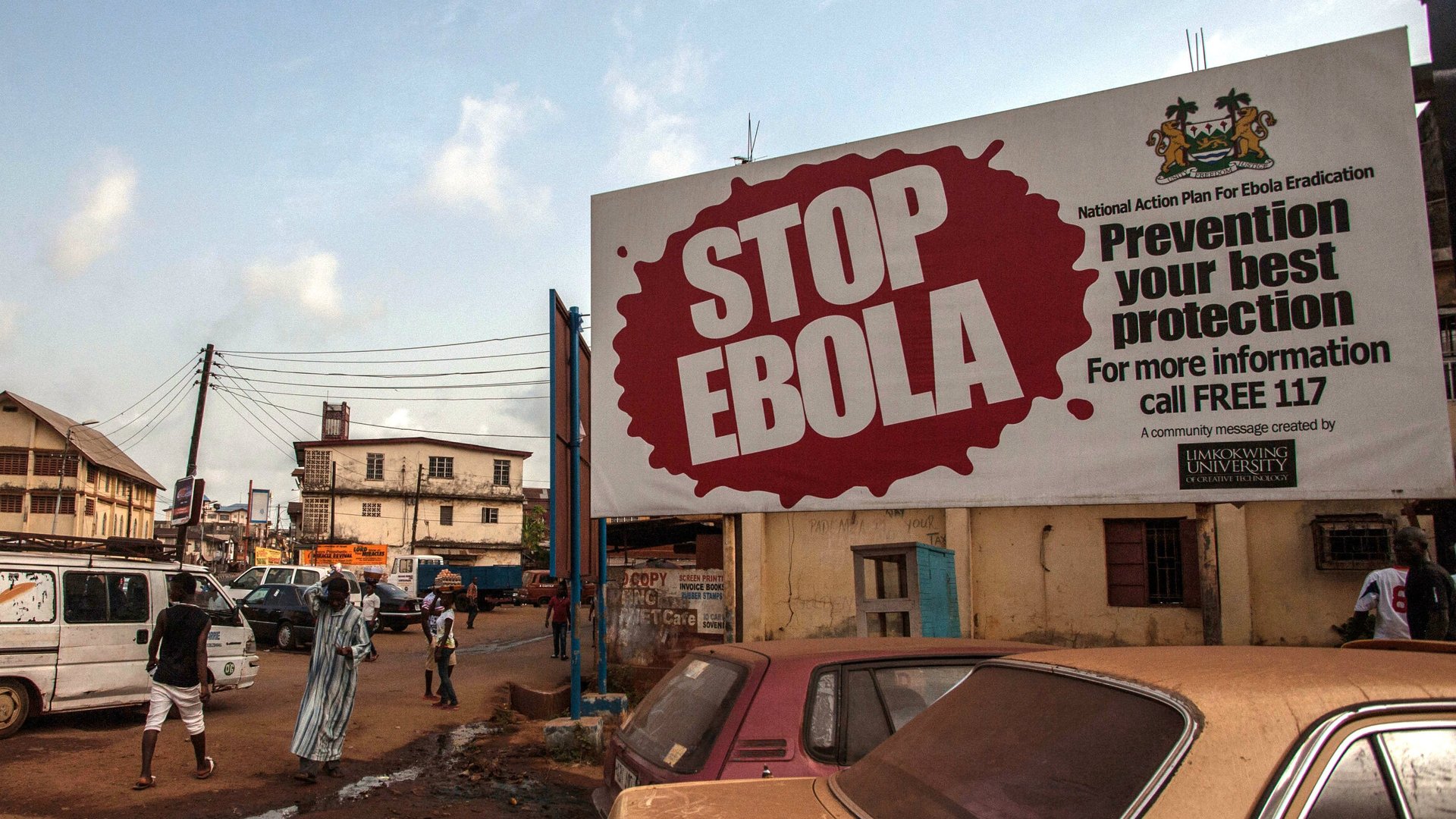
The lessons of West Africa’s Ebola’s crisis will save the continent from the worst of coronavirus
The Ebola outbreak across West Africa between 2013 and 2014 was devasting taking more than 11,000 lives in three countries. And yet, it could have been so much worse but for the heroic actions of Nigerian doctor, Ameyo Stella Adadevoh.


The Ebola outbreak across West Africa between 2013 and 2014 was devasting taking more than 11,000 lives in three countries. And yet, it could have been so much worse but for the heroic actions of Nigerian doctor, Ameyo Stella Adadevoh.
With the viral outbreak already taking hold across West Africa in Sierra Leone, Guinea and Liberia, the threat of a devastating outbreak loomed large in Nigeria—by far the region’s largest country. And it nearly proved to be the case but for Dr. Adadevoh’s selflessness. As part of the team that diagnosed, quarantined and treated Nigeria’s first Ebola patient in Lagos, Dr. Adadevoh helped contain what could have proved a deadly outbreak in Nigeria’s densely populated commercial center. Ultimately, it came at the cost of her life.
As African countries appear at risk of another viral outbreak with COVID-19 (as the particular coronavirus strain in China is now known), effective containment this time around will likely require more than valiant heroics. The World Health Organization and other regional and country public health experts are very worried the “fragile” health systems in most African countries will be unable to cope if coronavirus takes hold on the continent. Even China with its larger pool of technical and financial resources, appears to be struggling to contain the virus.
With nearly 5,000 African students studying in Hubei province where Wuhan is ground zero for the deadly virus and many more Africans living across China the continent’s risk of an outbreak is very real.
Yet, in dealing with a potential COVID-19 outbreak on the continent, the African countries most recently affected by a previous viral pandemic will be leaning heavily on the past to address the present.
The legacy of Ebola
More than 11,000 people died in Liberia, Guinea, and Sierra Leone alone during the 2014 Ebola outbreak. And the cost of the outbreak was also counted in economic terms with losses of roughly $1.6 billion. But in its wake, Ebola also left affected countries with increased knowledge bases of how to handle viral outbreaks.
“Our preparedness is based on the system we built after Ebola,” says Dr. Mosoka Fallah, acting lead of Liberia’s National Public Health Institute. “The national institute that’s now leading preparedness for coronavirus did not exist before Ebola,” he says. “The skill did not exist before, the knowledge did not exist before, the manpower did not exist before and the infrastructure did not exist before.”
The aftermath of Ebola now means West African countries including Senegal, Liberia, Sierra Leone, Cote d’Ivoire and Nigeria currently rank as better prepared for COVID-19 than richer countries with more sophisticated health systems, says Gyude Moore, fellow at Center for Global Development in Washington D.C and former minister for public works in Liberia.
Compared to 2014, there are already far more African countries capable of testing and diagnosing COVID-19 samples. Last week, the number of laboratories in Africa able to test samples of the virus had tripled with Ghana, Madagascar, Nigeria and Sierra Leone joining a short list that previously only included Senegal and South Africa. For its part, Fallah says while Liberia still awaits chemical testing components for its lab, it already has the infrastructure in place to test COVID-19 samples. It’s a crucial step in preparedness given the importance of early detection and monitoring during viral outbreaks.
Having tested health surveillance and tracking systems is also key. Nigeria’s wider health system has also stepped up in tracking persons believed to have come in contact with any viral outbreak’s patient zero thanks to the country’s Centre for Disease Control’s (CDC) established network for dealing with diseases like Lassa fever, yellow fever and polio, says Dr. Mcginger Ibeneme, unit head for Lassa fever at the Nnamdi Azikwe University teaching hospital in Nnewi, southeast Nigeria. “We were able to actively trace every contact as soon it was reported,” Ibeneme says of the Ebola crisis six years ago. “There was no magic, it’s not like we had a cure at the time but there a structure for surveillance in all the Nigerian states.”
People power
While infrastructure, medication and know-how are vital in dealing with pandemics, they only remain a part of the solution. As the Ebola outbreak proved, health systems and workers will invariably also rely on getting locals to adopt simple but crucial behavioral changes, including consistent hand washing and ditching self-medication practices.
Given how long the process of vaccine development takes, behavior changes remain a low-hanging fruit for containing outbreaks. “If you’re going to control the spread and the transmission, behavior changes are going to be the first and probably best line of defense because it’ll take a while before we can find medical intervention,” Moore says. “By the time you are able to develop a medical counter-measure, the virus would have done significant damage.”
But getting the message of behavior change across to locals is not so simple given cultural or even religious nuances.
Amid the Ebola outbreak in Liberia, with the government looking to get Muslims to stop handling possibly infectious corpses in the process of burial rites, it took the country’s head Imam going on national radio to discuss the issue before significant change was noticed. “The government could have gone on radio as many times as we wanted but it wouldn’t have been enough to alter people’s behavior,” says Moore, who was a government minister at the time. “It’s about finding repositories of trust and incorporating them into your incidence response system.”
Optimizing authority figures to get the message serves a double-purpose of changing social behavior and winning the public over as allies to supplement weak health systems especially where gaps in surveillance and patient tracking can worsen the outbreak, as seen in Sierra Leone. “The initial surveillance system in Sierra Leone was not enough to contain the disease and there was an escalation,” says Ibeneme who spent six months in the country as response team lead for the African Union. “That escalation made surveillance even more delicate for us.”
But with the need for possible behavior changes now better understood, especially in the countries worst affected by Ebola, chances are locals will now be far more receptive. And there’s already some early-day evidence to support that notion: “There’s more awareness and people are more proactive now,” Fallah says. “As bad as Ebola was, it was also a learning process and you can see that now.”
Getting set
Ultimately, not all African countries can reflect on direct Ebola lessons and suffering one viral outbreak doesn’t exactly render a country immune from another—as DR Congo’s 10th and ongoing Ebola outbreak shows. Given close travel and trade links to China, African countries still broadly remain at risk.
To ensure the best possible outcome in the event of an outbreak, African countries must prepare for the worst. “It’s better to over-prepare than to over-react,” Moore says. “In Liberia, we based our preparation on what we knew of outbreaks that had happened in the past and, when the outbreak exceeded anything that had happened before, we were grossly unprepared.” Where they don’t exist already, preparedness should begin with selecting sites and locations for temporary hospital set-ups to isolate and treat patients and kicking off awareness campaigns early, Moore says.
But given the reality of underfunded health systems across the continent, preparedness levels often mirror financial capabilities. And that’s where global bodies like the World Health Organization (WHO) matter. “Putting funding into this stage of preparation efforts across Africa will be the best investment at this stage,” Fallah says. For its part, WHO also has some learning to do in that regard having faced widespread criticism for its slow response to the Ebola crisis in 2014.

As African countries look to learn from what worked during the Ebola crisis, they can also learn from what didn’t, including quarantine methods. “We tried to quarantine entire communities like we see China doing now but that proved counter productive because you have to engage them,” says Moore. “You want the community to continue to retain its trust of the authorities so you have to act in ways that promote trust not undermine it.”
Just like during the Ebola outbreak, countries will likely be tempted to insulate themselves as an instinctive protective measure but the chances of ending the outbreaks hinge on collaboration rather than isolation, Moore adds: “These outbreaks end if the response is collective, not individual”
Sign up to the Quartz Africa Weekly Brief here for news and analysis on African business, tech and innovation in your inbox