90% of mpox deaths in the US have been Black men
The majority of victims were immunocompromised because of HIV
Between May 10, 2022 and Mar. 7, 2023, more than 30,200 people in the US contracted mpox (formerly: monkeypox). The majority of cases occurred between the end of June 2022 and early September 2022, though new infections were recorded as recently as the week of Feb. 26, 2023.
The mortality rate of the disease has been measured as 1.3 per 1,000 cases, slightly higher than the global 1.2 per 1,000 cases. In the U.S., 38 deaths have been recorded, mostly between mid-September 2022 and the end of the year. According to data released on Apr. 14 by the Centers for Disease Control and Prevention (CDC) the median interval between symptoms onset and death is 68 days, with a range between 58 and 86 days.
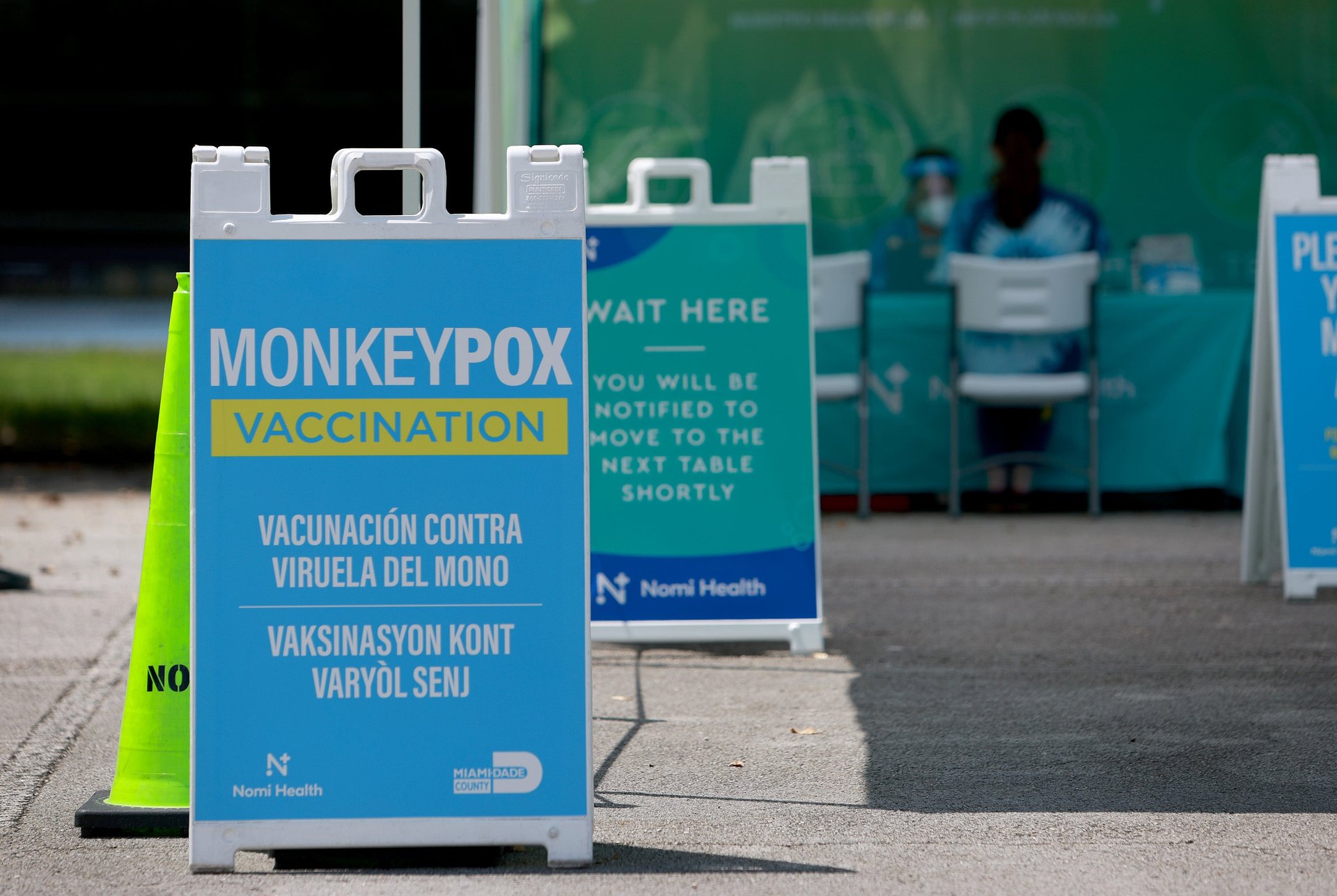
Much like previous outbreaks, mpox—which shows a discrepancy between who was getting infected (mostly Black men) and who received mpox vaccines (mostly white men)—is a picture of inequality.
A shocking discrepancy
When it comes to race and ethnicity, the disproportion in mpox outcomes is striking. In the interval analyzed by the CDC, deaths from mpox in the U.S. were extremely concentrated: Nearly 90% of them occurred among Black people, and 95% of the victims were cisgender men. Black people, who represent about 13% of the population, accounted for 33% of the cases and 87% of deaths.
The discrepancy mirrors the current perception of the mpox emergency. The CDC has stopped sharing weekly updates with case data, and the emergency is often discussed as past. “I think we always have to ask who the emergency is over for,” says Joseph Osmundson, a professor of biology at New York University and a queer health advocate. “I know for a fact that there are Black men in a hospital in New York City right now fighting for their lives who are likely to not make it.”
There are two things pretty much all people who died for mpox-related causes had in common: They were Black men, and they were immunocompromised because of HIV.
Having mpox while Black
Rico Lee, a cardiac monitor technician based in Atlanta, Georgia, is not surprised by the finding. As a Black, gay man, his experience trying to get treatment for an increasingly severe case of mpox was an ordeal that took four emergency room visits and two doctor consultations.
On Aug. 1, 2022, Lee woke up with what looked like a pimple on his face. He tried to treat it with an over-the-counter product, but it didn’t go away, and several others soon appeared. Lee was aware of an mpox outbreak in Atlanta, and he knew that his immunity was likely compromised because of his recent covid infection. He’d received the first dose of mpox vaccine only a couple of days prior—not enough to provide him with immunity. He had tried to get it sooner but, despite belonging to a target group for mpox prevention, it took a month before he resorted to getting one an hour’s drive away.
Lee visited the emergency room at a local hospital, where doctors diagnosed him with mpox visually, administered a test, and sent him home, recommending that he treat his symptoms with over-the-counter medications. A week later, the test results confirmed he had mpox. Meanwhile, the sores had grown more numerous. Lee had developed fever of 104.4° F (40° C) and could barely swallow. As a trained nurse, he recognized the signs of a worsening viral infection and went back to the ER.
“They told me to go home, stay hydrated, take Tylenol and ibuprofen every so many hours, and that was that—let it ride out because it’s a virus,” says Lee. He was not given tecovirimat (tpoxx), the smallpox drug used to treat mpox. When the symptoms kept worsening despite the over-the-counter medications, he reached out to his doctor via a telehealth visit. The doctor tried to prescribe tpoxx but was delayed as he waited for approval from his manager.
Meanwhile, Lee’s symptoms were worsening. After he fainted in his apartment, he returned to the ER a third time, where he was given fluids and told to take an allergy medication. He soon realized his heart was racing.
“I told [the doctor] ‘Hey, my heart is racing really fast. I think this might be considered supraventricular tachycardia,’” says Lee, who as a cardiac technician is familiar with heart conditions. “She looked at me as if I didn’t know what I was talking about.” When the doctor refused to check his heart, Lee used an app on his phone to show her his heartbeat was above 200 beats per minute. The doctor gave Lee an EKG and diagnosed him with supraventricular tachycardia.
After being given treatment for his irregular heartbeat, Lee was again sent home with the assessment that it was his being overweight—not the high fever—that caused the cardiac issue. Meanwhile, his primary care doctor’s request for tpoxx was denied on the basis that Lee didn’t have enough risk factors to develop a severe case of mpox—despite the fact that his symptoms had been worsening for weeks.
As the high fever and brain fog continued, the sores on Lee’s face began breaking. “My face [was] opening up, my skin smell[ed] like rotting flesh,” he says. He recognized that he might have cellulitis, a potentially fatal bacterial skin infection he recognized from treating patients with it. He went back to the ER one last time, where the same doctor who had refused to take his EKG tried to send him home, again blaming his being overweight for the complications he was experiencing. But Lee refused to leave, leaning on his nursing training to demand specific treatments for cellulitis and other symptoms. He succeeded, and within a week, his face began healing—though the scarring is permanent. He knows others haven’t been as fortunate.
“My heart goes out to those Black men who died because they couldn’t advocate for themselves and were turned away,” Lee says.
The link to HIV
Mpox deaths typically occur in people with compromised immunity. The latest CDC data confirms it: All the victims for which information was available were immunocompromised, 94% of whom were HIV positive and not on anti-retroviral drugs.
“The case reports of advanced HIV and mpox are just almost too hard to read,” says Osmundson, the NYU biology professor. “It’s fingers falling off, it’s so many lesions on the throat that the patient has to be intubated, it’s tpoxx failing orally because the patient can no longer swallow, so the drug has to be given intravenously. It is just so harrowing.”
There is a parallel between mpox and HIV. At this point—particularly in the US where Pre-Exposure Prophylaxix (PrEP) and antiretroviral drugs are supposed to be widely available—the HIV emergency is largely a thing of the past. Yet while 67% of white people who are eligible for PrEP are on it, only 8% eligible Black people are, often citing lack of access to healthcare or to compassionate healthcare.
The fact that mpox deaths were mostly among HIV-positive people suggests that the same group of people who is failed by AIDS prevention and treatment strategies was failed by mpox vaccination initiatives, says Osmundson.
“We always knew who was going to die,” he says. “Thirty deaths of Black men are not acceptable. They were preventable.”
