A new Sickle cell disease drug holds much promise but most sufferers won’t be able to afford it
The regulatory approval of a groundbreaking new Sickle cell disease drug in the United States by the Food and Drugs Administration (FDA) sparked off plenty of hope and optimism earlier this month and the news that it is already heading for clinical trials in some African countries was also welcomed.
The regulatory approval of a groundbreaking new Sickle cell disease drug in the United States by the Food and Drugs Administration (FDA) sparked off plenty of hope and optimism earlier this month and the news that it is already heading for clinical trials in some African countries was also welcomed.
But that optimism has been replaced by concerns the new treatment is priced beyond the reach of the majority of sufferers on the continent.
Swiss pharma giant Novartis announced this month the US FDA approved its new drug crizanlizumab, marketed as Adakveo, for adults and patients over 16 to start using the medication in a matter of weeks. In recent years Hydroxyurea has been the standard-of-care drug for the treatment of sickle cell disease’s pain crisis.
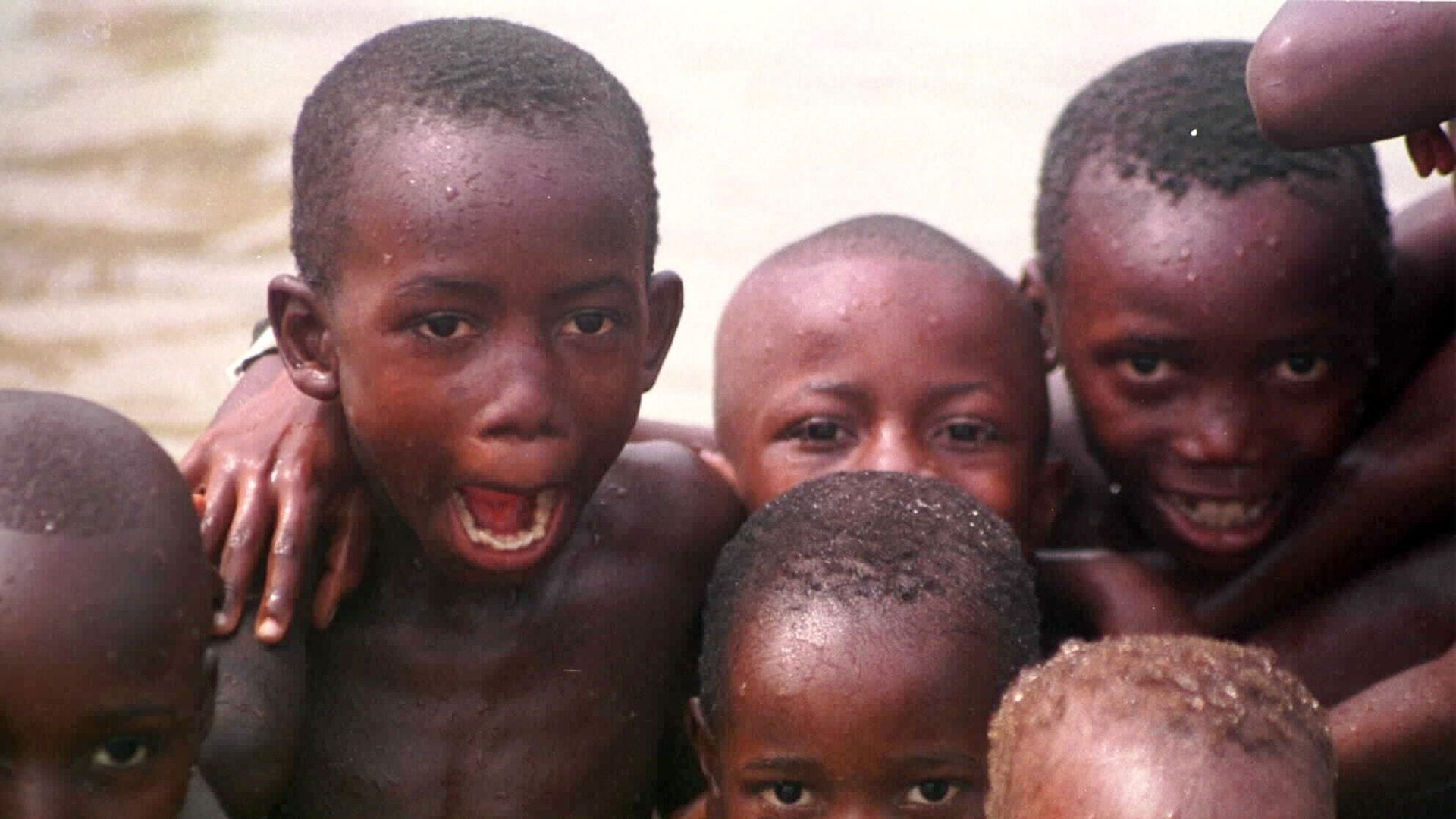
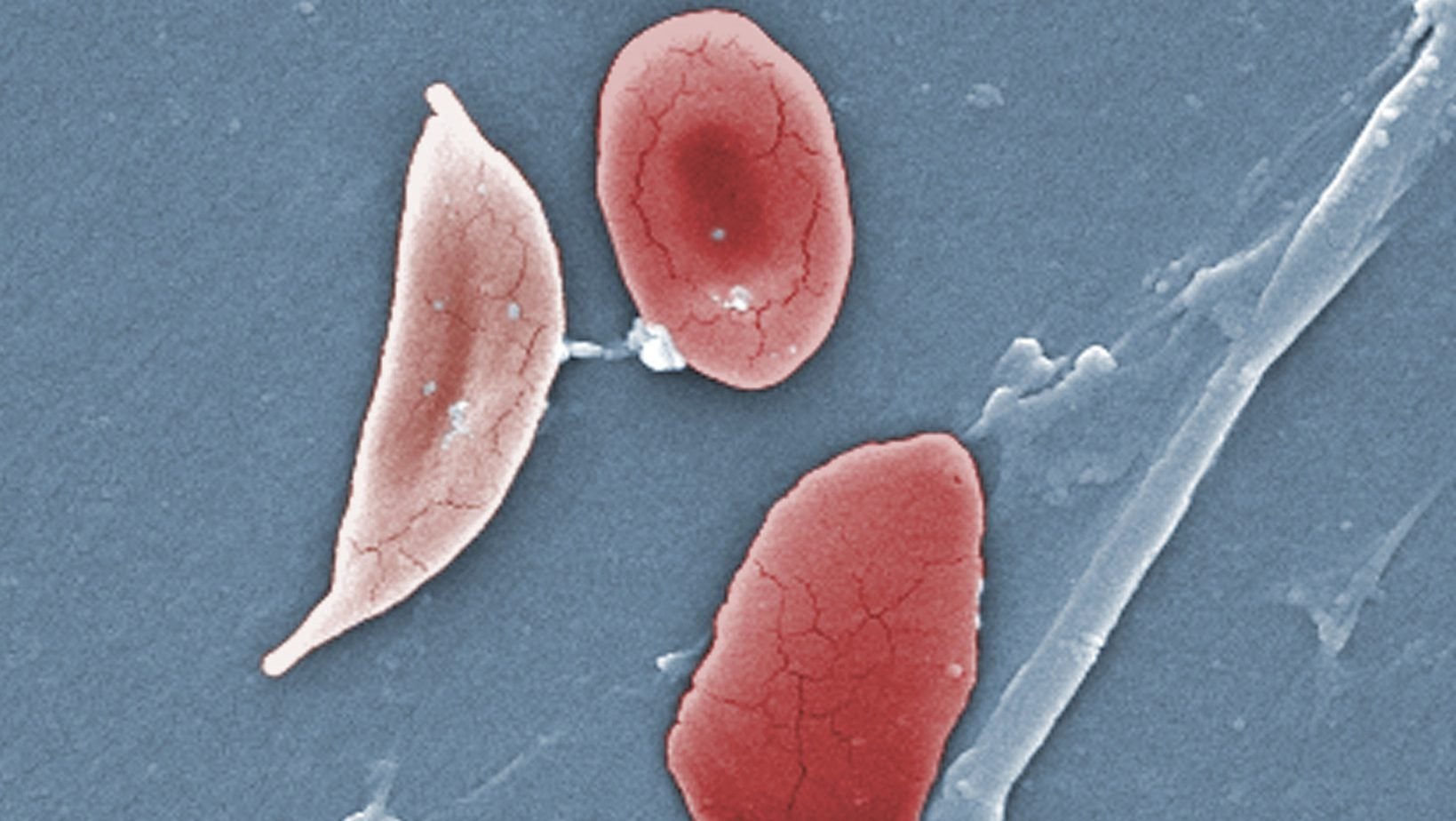
Sickle cell disease, which is also known as Sickle cell anemia, is an inherited red blood cell disorder which affects over 12 million people, mostly with origins in sub-Saharan Africa, India, Saudi Arabia and Mediterranean countries The disease is regarded as a silent baby killer as an estimated 50% to 80% of infants born with the disorder die before the age of 5 years. Each year about 300,000 infants are born with major sickle-cell disorders—including more than 200,000 cases in Africa, according to WHO.
A sickle cell patient can suffer intermittent extreme body pain commonly referred to as a “crisis” due to the “sickling” of some red blood cells.
Adakveo is said to work by reducing the annual rate of sickle cell pain crisis by 45%. It was also reported to have reduced hospitalization and nearly four in ten patients who received the new treatment were said not to have experienced any pain crisis.
However, to achieve these best-case results from the new drug, a healthcare worker would need to administer up to four vials each month to each patient as infusion, Novartis says. This is in sharp contrast to hydroxyurea which is available in capsules and does not require hospital visits that would be additional costs for patients.
Novartis also revealed that annually, the new drug will cost between $84,852 and $113,136. In the US alone, the pharmaceutical giant has said it expects to generate more than $1 billion from the drug, largely from Medicare, Medicaid and other government payers as well as private health insurers.
African reality
But even though Sub-Saharan Africa accounts for the highest disease burden and, according to the WHO, sickle cell disease affects most countries in the African region, the underfunded health systems of most countries in the region are unlikely to be able to subsidize the cost of the drug for patients.
The dominance of out-of-pocket as the major method of payment for healthcare services in African countries means the drugs will be out of reach for the majority of people who need it the most.
In comparison Hydroxyurea is taken once daily and 100 capsules are sold for $78, putting an individual’s annual cost for the drug at around $300. While comparatively lower than the cost of Novartis’ latest drug it is still very expensive for many individuals with sickle cell disease in countries like Nigeria and is a leading reason for non-compliance among many patients with the disease.
In spite of the numerous challenges of African markets, Novartis told Quartz that if approved, Adakveo can play a role in reducing the burden of sickle cell pain crisis in Africa and is already in talks with authorities about pricing.
“We are in the process of registering the medicine with other health authorities globally; this process includes discussions on pricing,” a Novartis spokesperson says.
To better understand how to introduce the new drug in Africa, the company said it is planning to hold multicenter clinical trials in sub-Saharan Africa in 2020. The trials will be conducted at sites in Ghana and Kenya.
“In order to bring any new therapy into developing countries, we must first help ensure the healthcare systems are ready to receive it,” the company adds.
Novartis will be hoping to gain adequate ground in the market before Voxelotor, a once daily pill from Global Blood Therapeutics Inc, gets FDA nod early next year, and the controversies surrounding Niprisan, a Nigeria-made phytochemical indicated for reducing the occurrence of sickle cell crises, are resolved.
Sign up to the Quartz Africa Weekly Brief here for news and analysis on African business, tech and innovation in your inbox