Coronavirus: Just the vax, ma’am
Hello Quartz readers,

Hello Quartz readers,
While many people wait to find out when they can leave their homes, a select few are awaiting news on when they can leave the planet. Yesterday, weather concerns forced NASA and SpaceX to postpone the first crewed flight of a spacecraft to orbit from the US since 2011.
Leaving Earth entirely, however appealing, is no cure for coronavirus. But as the global economy reels, it’s a reminder that the future could still bring prosperity and innovation. SpaceX’s Crew Dragon is the first human-carrying orbital spacecraft designed by a private company—ever!—and it may be the cheapest ever made. As Quartz’s Tim Fernholz wrote, that could signal “a paradigm shift that promises a whole new world of economic activity in space, with private organizations doing what once required an entire nation.”
Back on solid ground, all eyes are on a different race: the one for a coronavirus vaccine. We’ve gotten a lot of questions on this topic: How do vaccines work? When will we get one? Why is this taking so long? Today we’re diving into them. Let’s get started.
Post-Moderna
There are currently more than 140 Covid-19 vaccine candidates in development. At this early stage, tracking their slow progress probably isn’t worth much of your time—unless, that is, you’re an investor in the pharma companies promoting their results.
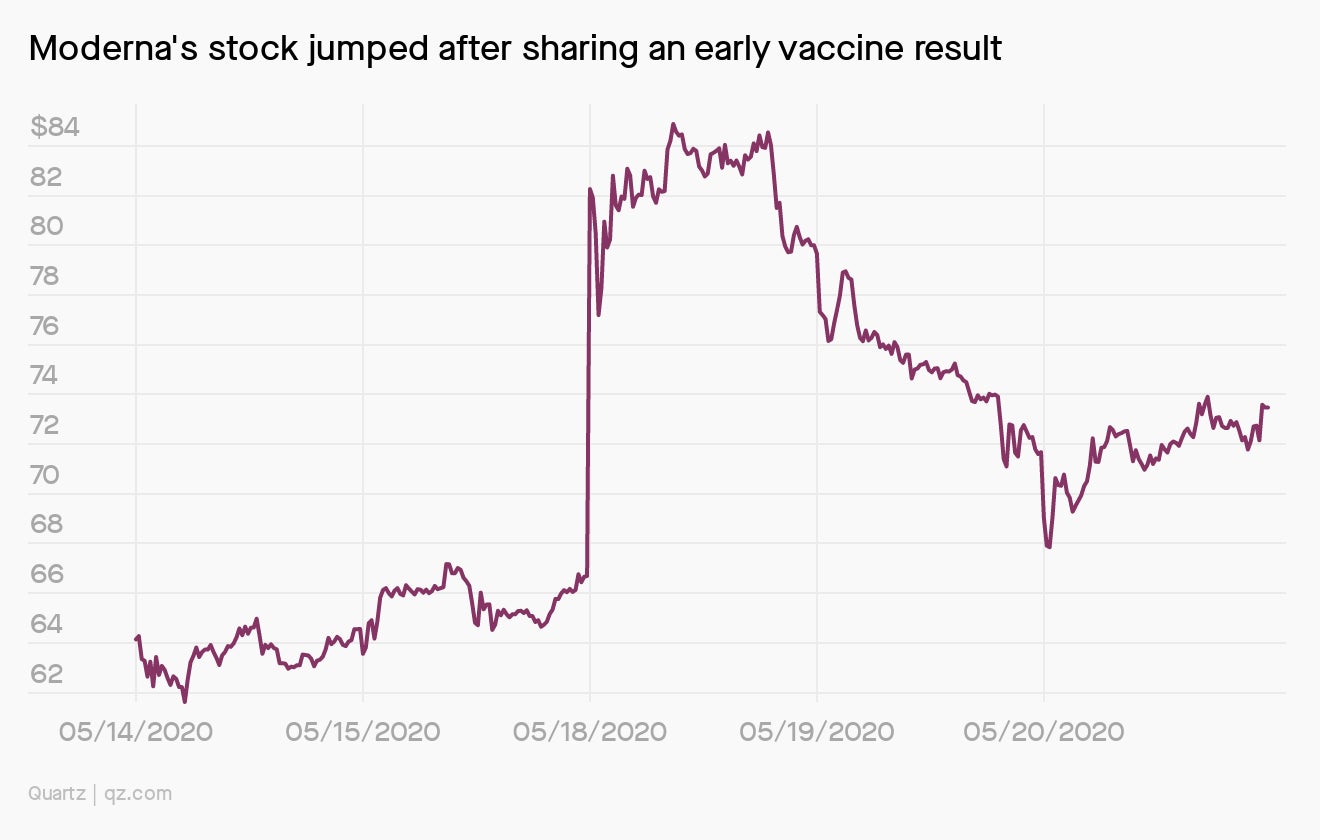
Last week, Massachusetts-based Moderna announced results from a phase I trial of one such vaccine. This was just an initial safety test of a new concoction: The trial had only 45 participants, eight of whom developed the neutralizing antibodies against SARS-CoV-2 that theoretically confer immunity. Stocks rallied in response.
Normally, such small safety trials aren’t much to get excited about. It typically takes months or years to conduct the follow-up phase 2 trials (does the drug actually work?) and phase 3 trials (does it work in a large group of people?) that can lead to approval from the US Food and Drug Administration.
But this time is different: The FDA has said it would authorize the use of vaccines for limited populations before approval, so every trickle of data is being taken seriously. That makes even small trial victories definitive wins for certain companies’ investors. Moderna shareholders include former GlaxoSmithKline vaccines chief Moncef Slaoui, who is the new leader of a US program to speed vaccine development. (Slaoui must dump 155,000 Moderna shares to take the job.) This week, STAT reported that Moderna’s chief medical officer has since February liquidated all of his shares—for $18 million in profit.
Mass-producing a single vaccine for immediate use around the world would be impossible with current manufacturing capabilities. Our best chance to provide global access to a Covid-19 vaccine is actually to have several (Quartz member exclusive). Which means we can expect plenty of market peaks and valleys as dozens of companies release early-stage results.
Antibody building
Pharmaceutical companies are developing potential vaccines in a few different ways, each requiring its own set of specialized equipment. But all of these vaccine types have one thing in common: They function as biological catfish (the MTV-show kind, not the freshwater kind). That means they trick your B-cells, a type of immune cell, into making antibodies against a pathogen—something B-cells normally do only if there’s an infection present.
How to convince your body there’s a baddie around when there really isn’t? To explain, let’s pretend that the SARS-CoV-2 virus is a villain with a signature lewk, like, uh, Darth Vader.

Weakened or inactivated virus vaccines take copies of a virus and physically or genetically modify it so it’s harmless. This would be like disarming Vader by taking away his lightsaber or turning off one of his breathing devices. He’s suddenly just an old man that can’t do your body any harm, but he looks threatening enough to trick your B-cells.
Subunit vaccines replicate a signature part of the virus. For SARS-CoV-2, that’s the S-protein it uses to enter our cells. For Vader, it’s his helmet. These vaccines essentially tell B-cells, “If you see anyone wearing this helmet, they’re an infection.” The helmet on its own can’t hurt the body, of course, but it’s still enough to get the B-cells moving.
Virus-like particle vaccines are a type of subunit vaccine, but take a slightly different approach: They mimic the virus’s outer shell, aka Vader’s signature cape and black boots. Like other subunit vaccines, they communicate that anything wearing this particular outfit is Bad News, and that it’s probably time to deploy some X-wings (antibodies).
Viral vector vaccines also trigger B-cells with a signature protein, like Vader’s helmet. But rather than build a whole helmet assembly line, they use a benign virus (the vector) to carry the genetic instructions for that helmet into our cells. Once inside, they co-opt our cells’ hardware to mass-produce the helmets, which our antibodies learn to recognize and destroy.
Nucleic acid vaccines, like Moderna’s, also get our cells to do their dirty work. These vaccines insert viral genetic information into our cells directly, instead of using a viral vector. It’d be like placing holographic instructions to make Vader’s helmet inside a rebel droid. No nucleic acid vaccines have ever been approved—but there’s a first time for everything.
A version of the above first appeared in Scrap Facts, a newsletter from Quartz health reporter Katherine Ellen Foley. She used the example of Yzma, a villain from The Emperor’s New Groove, but we made her age up the reference.
🏖️ More than a fling 🏖️
Summer 2020 is for cutting things in half: your travel budget, your pant legs, and the cost of a Quartz membership. With this 50% discount, you can enjoy full access to our in-depth field guides, award-winning reporting, and other member perks. Here’s some of our favorite member-only content from this week:
- What will it take for Netflix to fail during a pandemic?
- TikTok users are gaming China by praising China
- Sci-fi authors predicted the future, but it arrived ahead of schedule
Rising to the challenge
Usually, testing a vaccine means injecting thousands of people with either the drug or a placebo, then waiting months or years to see who gets sick. We don’t have that kind of time. So instead, scientists and ethicists are debating whether to set up challenge trials: deliberately exposing a few hundred people to SARS-CoV-2, only some of whom receive a vaccine.
This is obviously risky: Any participant could get a potentially fatal infection. To try to avoid this, scientists would recruit only the youngest and healthiest volunteers—but that would mean that the vaccine wouldn’t be validated for use in some of the older or otherwise more vulnerable populations. To minimize risk, scientists would also have to figure out a dosage of the virus that causes infection, but is less likely to cause severe reactions.
A fast turnaround trial like this could also be risky for future vaccine recipients. It won’t be able to tell us whether a vaccine produces long-term side effects. Ideally, scientists could wait months or years before evaluating the safety of the vaccine, lest we see another iteration of a hastily-developed 1976 flu vaccine. That vaccine, created after a small outbreak of the virus, ended up causing severe nerve complications in some of the people who received it.
So far, over 10,000 people have said that they’d participate in a challenge trial. Would you?
You asked
If we are able to develop a vaccine, will vaccinated people who later get exposed to the virus still be able to pass it on to other, not-vaccinated people?
Great question, Petra. While viruses can survive on skin or other surfaces for a short time, they can’t replicate outside of cells. The process of replicating is what causes infections, and what allows the virus to spread from person to person.
When someone has recovered from an illness or gotten a vaccine, they have antibodies against the virus. If they encounter it again, their bodies have a built-in defense system—without a home, the virus dies off. When enough people can’t host the virus, the whole community is protected against it; this is what immunologists call “herd immunity.”
All of which is to say that a person who has been vaccinated shouldn’t be able to transmit the virus to someone who hasn’t been vaccinated, because they can’t host a virus long enough for it to replicate. That said, if a vaccinated person has a virus on their hands and touches another person without washing them, they could pass it on. Good personal hygiene is always a great defense against infection.
Essential reading
- The latest 🌏 figures: 5,936,145 confirmed cases; 2,389,056 classified as “recovered.”
- Weakened work: Post-outbreak, China’s young struggle to find jobs.
- The loan danger: A fraction of the Fed’s lending facilities have been tapped so far.
- Perk from home: What will happen to lavish office perks?
- Cyberse-cure-ity: Hackers are pivoting to medical espionage.
Our best wishes for a healthy day. Get in touch with us at [email protected], and live your best Quartz life by downloading our app and becoming a member. Today’s newsletter was brought to you by Katherine Ellen Foley, Olivia Goldhill, Katie Palmer, Susan Howson, and Kira Bindrim.