India’s Covid-19 horrors played out in many parts of south Asia this year
Over the last two months, as India dealt with one of the world’s deadliest Covid-19 waves, a host of its neighbours suffered a similar plight.


Over the last two months, as India dealt with one of the world’s deadliest Covid-19 waves, a host of its neighbours suffered a similar plight.
From a sharp increase in new coronavirus cases to record high positivity rates, and insufficient healthcare infrastructure, most south Asian countries have had a bitter experience with Covid in recent weeks. In some regions, the outbreak was directly linked to India.
On May 25, south Asia was recording over three new Covid-19 infections every second and one death from the disease every 17 seconds, according to the UNICEF.
“The scenes we are witnessing in South Asia are unlike anything our region has seen before,” George Laryea-Adjei, UNICEF’s regional director for South Asia, said on May 25. “Family members of patients are carrying oxygen cylinders inside hospitals, risking their own lives in hopes of saving a loved one. Exhausted health workers are working sixteen-hour days, unable to pay individual attention to every patient under their care. We are faced with a real possibility of fragile health systems collapsing.”
Here’s a look at how the Covid-19 crisis played out in the south Asian region:
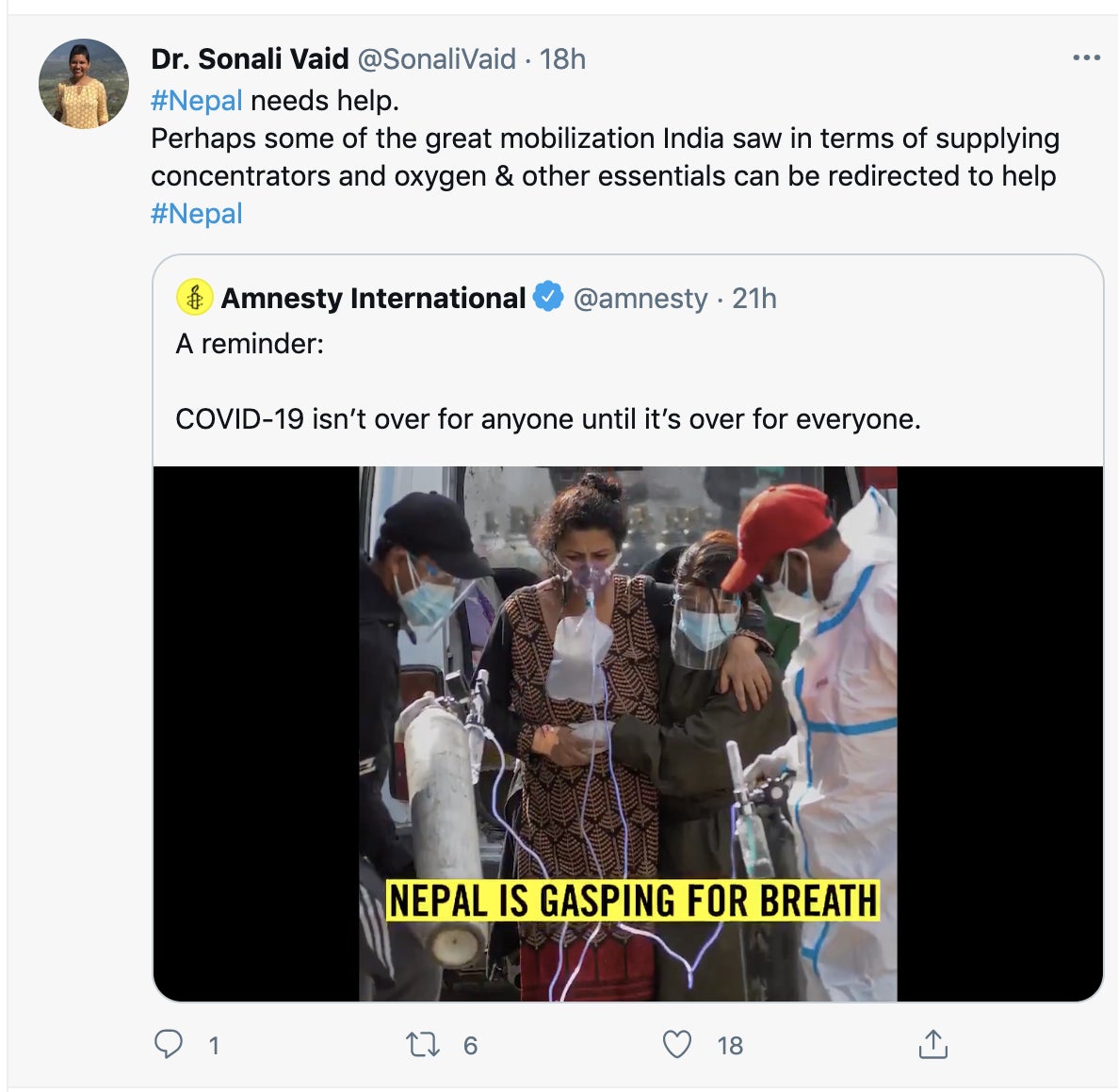
Nepal’s Covid-19 surge and its India connection
Nepal, which shares a 1,850-kilometre border with five Indian states, witnessed a runaway second wave in May.
The Himalayan country went from reporting 100 new cases daily in early March to over 9,000 by late May. The country’s positivity rate—the share of tests that come back positive—reached a staggering 47% during the month. And on a per-person basis, Nepal’s Covid surge exceeded India’s.
Nepal and India’s fates are intertwined due to the constant movement across their border. When India’s second wave began in early April, thousands of Nepali migrant workers fled to their home country. This continued to happen despite border closures.
In addition, in April, Nepali Hindus travelled to Uttarakhand in India to attend the super-spreader religious event Kumbh Mela. The country’s former king and queen, two of the 9.1 million devotees in attendance, tested positive upon their return.
A lab that did genomic sequencing of a dozen samples in the Kathmandu Valley in late April and early May found that 11 of them were versions of the variant first identified in India.
Mirroring India’s brittle healthcare system, Nepal’s hospitals struggled to deal with the situation. ”Right now, there are no beds available today in any hospital that is treating Covid patients,” Jyotindra Sharma, a Kathmandu-based doctor, told India Today in mid-May. “Even if there are any beds, there is a huge scarcity of oxygen. The supply of oxygen is a major problem to take new patients. And we are not even at the peak of this wave.”
The number of daily Covid cases in the country is currently much lower than the peak in mid-May.
Sri Lanka’s Covid struggle
Sri Lanka witnessed a surge in coronavirus cases in May, the month after two major festivals, Sinhala and Tamil New Year, when people thronged markets and gathered to celebrate. Once the numbers began escalating, the Sri Lankan government issued a five-page guideline to limit movement, but it was widely criticised for lacking clarity and cohesion.
At the end of May, nearly nine in 10 hospital beds in the country were in use.
The country’s second wave began towards April end and is still continuing. On June 9, Sri Lanka reported 66 deaths due to Covid-19, its highest single-day tally.
Maldives’ coronavirus mishaps
For a while, Maldives appeared to be a safe haven. A favourite holiday destination for affluent Indians in the midst of the pandemic, at least a dozen Bollywood actors and thousands of Indian tourists flocked to Maldivian resorts for much of 2020 and early 2021. With stringent testing to enter and exit the island, authorities managed to keep the situation in check for a while.
However, in April, the island nation bore the brunt of violating social distancing norms amid local elections and Ramadan celebrations.
By the end of April, Maldives imposed a strict curfew from 4pm to 8am in a bid to stop its healthcare workforce from getting overwhelmed. “Especially due to the situation in India, which is traditionally the biggest source country, we are finding it difficult to hire new medical professionals to deal with the increased caseload,” Mabrook Azeez, the spokesman for the President’s Office told Reuters. On May 13, the island banned Indian tourists.
The country has seen a steady decline in cases in June so far.
Covid in Pakistan, Bangladesh, and Afghanistan
India’s other immediate neighbours have also faced a tough time.
In mid-April, the total number of critically ill coronavirus patients on oxygen in Pakistan reached 5,360, 57% more than the peak last June. Bangladesh went into lockdown for over a month starting April 5 amid fears of a looming outbreak. The healthcare infrastructure of both countries was at full capacity by May. While cases have dropped, experts warn both Pakistan and Bangladesh may be easing restrictions too soon. The latter is already paying the price with infection rates nearly doubling from 7% in early May to over 13% on June 10.
In Afghanistan, infection and death rates are currently surging. The government has neither restricted mass gatherings in most cases nor put a stop to travel from India. Masks have been a rarity and myths about the reality and gravity of the virus are aplenty. “Our people believe it is fake, especially in the countryside,” said Zalmai Rishteen, the hospital administrator at the Afghan-Japan Hospital. “Or they are religious and believe God will save them.”
Covid and the rest of south Asia
A little farther from India’s borders, too, the situation remains grim.
In early May, there was a mad scramble for medical resources in the Philippines. In Thailand, where there was a paucity of beds and oxygen in the country in mid-May, patients had to be crammed into makeshift facilities student dorms.
By May-end, Malaysia was posting a five-fold increase in cases compared to two months ago. The country went into a 14-day lockdown on May 28, which it will likely extend. Sepang-headquartered AirAsia has grounded 90% of its fleet.
Around the same time, corruption and poor governance caused a resurgence of the virus in Cambodia. Weeks later, cases are still rising in the country.
In Taiwan, previously heralded as the exemplar of curbing Covid-19, prevention fatigue has led to an uptick in infections in recent weeks.
Indonesia is witnessing a surge in cases this month, right after there was a lot of activity for Idul Fitri. It posted the highest rise in cases in three months on June 9.
While social distancing and ramping up healthcare infrastructure are the need of the hour, there’s one common thread tying all of these countries in distress together: Their obtuse vaccine rollout.
A fraught vaccine rollout
Vaccination drives in the south Asian countries witnessing a surge in Covid-19’s resurgence are pitiful.
The processes are often scattered and vaccine equity is lacking. Adding to the trouble vaccine hesitancy is rampant in many parts of the region. Local governments in Pakistan are even passing orders to withhold salaries and block SIM cards of people who refuse to get vaccinated in a bid to encourage inoculation.
So far, all of them have vaccinated less than 5% of their population, barring Maldives and Cambodia.
While India has started reporting less than 100,000 cases now—down from a peak of over 400,000—it surely isn’t out of the woods. There are multiple variants of coronavirus in the country, some more concerning than others. Meanwhile, as states start easing lockdowns, Indians are still wearing masks incorrectly and crowding. Experts have warned that a third wave is inevitable.
The biggest black spot for the country is its vaccination process. For one, there are massive supply constraints. Secondly, there are technical snags with the appointment booking platform. Then, the distribution of vaccines has changed hands from central to state governments and back to the centre, with many hiccups. On top of all these missteps, vaccine pricing has been another point of contention.
In fact, the vaccination plans of several of its neighbours have been crippled because of India. Pakistan, Nepal, and Bangladesh were among the 91 countries that faced shortages after India halted exports of vaccines manufactured by the Serum Institute of India in March.
Other channels like the World Health Organisation’s Covax programme for low-income countries have been inefficient, too. For instance, Afghanistan was due to receive three million doses from this route in April, but they won’t arrive until August.