In 1992, the New York Times published an editorial (paywall) on the importance of promoting breastfeeding in the developing world. A reader—and health care worker—responded by writing in a letter to the paper voicing a then-common argument in support of breastfeeding.
“As long as children are breastfed, the holding, cuddling, and skin-to-skin contact they receive with their feedings eliminate the disparities between rich and poor,” New Jersey nurse and lactation consultant named Charlene Stokamer wrote (paywall).
Twenty-five years later, the American Academy of Pediatrics (AAP) advises that infants consume nothing but breast milk for the first six months of life and continue to breastfeed until at least their first birthday. Breastfeeding, the organization said when reaffirming its guidelines in 2012, “should be considered an investment in the short- and long-term health of the infant, rather than a lifestyle choice.” American parents have listened: more infants in the US are now breastfed than at any time in the last 40 years.
Yet the dream of breastfeeding as the great equalizer hasn’t quite materialized. The children of well-off, well-educated mothers are far more likely to reach that six-month target—and to be breastfed at all—than babies born into less-privileged homes.
Well-off parents have access to the infrastructure that supports breastfeeding: longer maternity leaves, jobs that allow for pumping breaks, the ability to hire outside help to support a new mother, and—perhaps most importantly—immersion in a culture that unconsciously views breastfeeding as a desirable status symbol and pressures them to continue to that hallowed six-month mark and well beyond.
Breast milk has become a luxury good, another example of what the sociologist Elizabeth Currid-Halkett calls inconspicuous consumption: the investments in intangibles like health and education that increase social capital for the modern wealthy. And because these costs are largely invisible, it’s easy to frame breastfeeding as a free good equally available to all. The truth is much more complicated.
Breastfeeding goes from second-tier to socially desirable
“Breast is best” has not always been the mantra of the upper classes in the US. While the cultural definition of the “best” food for babies has fluctuated over the last century between infant formula and breast milk, one thing has remained constant: the most socially desirable form of infant nutrition has been whichever is harder for poor parents to access.
“Much of it has been a function of what costs the most. This can be terms of dollars or, as it is now, in terms of time,” says Currid-Halkett, a professor of public policy at the University of Southern California and author of the book The Sum of Small Things: A Theory of the Aspirational Class.
During the consumer-goods boom of the mid-20th century, infant formula—with its aura of scientific superiority and costly price tag—was the preferred feeding method for upper-middle-class families in the US. That began to shift in the 1970s, with a resurgence of interest (primarily among educated white women) in natural childbirth and breastfeeding. Advocates viewed the movement as a way to reclaim an empowering experience for women from a medical industry that prioritized doctors’ needs over those of mothers and babies.
Today, disposable income makes it easier to buy the accessories that alleviate the discomfort of breastfeeding: the Boppy pillow, the nipple shields, the gooey anti-chafing ointments. But nothing is as helpful to starting and maintaining breastfeeding than a woman’s time. That becomes clear when you look at breastfeeding rates and mandated weeks of paid maternity leave in different wealth countries:
Breastfeeding and maternity leave
Source: Save the Children (pdf)
The more time a woman has at home with a baby on maternity leave, the more likely she is to breastfeed. What’s more, the body’s production of breast milk operates on a “use it or lose it” principle. Women who still want to provide breast milk after they return to work (which, for most working US women, is well before the six-month mark) need to stop and pump throughout the day at the same intervals at which a baby would eat in order to maintain their milk supply.
The Affordable Care Act mandates that insurance plans cover breast pumps, and that US employers allow mothers of children to take breaks to pump at work for up to a year after birth. Still, pumping is inconvenient in the best of cases, and in others—like for women with jobs in the services or in transportation or really anywhere without the relative privacy of an office—it’s virtually impossible.
“Some of the mothers I work with don’t feel they can ask for the time” at work to pump, says Christine Mirzaian, a pediatrician and director of the AltaMed Lactation Clinic at Children’s Hospital Los Angeles. “Ultimately in order to sustain breastfeeding, [what matters is] the support that they receive from their family, from their partner, and for those returning to work, the ability to pump in their workplaces.”
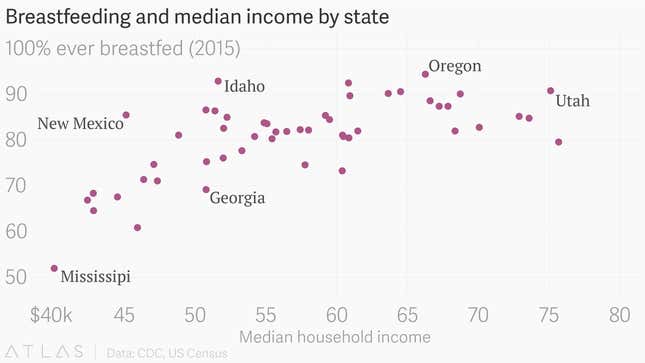
In the US, in states where median household income is lowest—and where more new mothers are more likely to work jobs outside of an accommodating office environment—rates of breastfeeding are also typically lower:
In The Sum of Small Things, Currid-Halkett argues that as the middle classes have become able to more easily obtain consumer products thanks to automation and globalized manufacturing, elites have shifted their consumption patterns to more subtle status markers that enhance knowledge, health, and—above all—their time. Time is a luxury good, and elites’ ability to enhance and prolong it only expands the inequality gap.
“The thing we lose sight of is that even though [breastfeeding’s cost] is not visible, it costs so much more,” she says. “The number of hours used to breastfeed a child for the year via AAP’s requirements is—I don’t even know how many thousands of dollars of a woman’s time that is.”
(Quartz did the calculations. For a woman making $60,000 a year pre-tax, working 50 hours per week, the monetary value of the time spent breastfeeding in the first six months—based on the average number and duration of daily feeds—is $14,250.)
Because the costs are not visible, it’s easier for people to tacitly judge a woman formula-feeding a young baby in a way they wouldn’t dream of doing if the woman was pushing the baby in a second-hand stroller. Without even being conscious of it, society has come to view breastfeeding as a status symbol.
The (marginal) health benefits of breastfeeding
The more breastfeeding rates stratify along class lines, the harder it is to objectively analyze its benefits. To be sure: science has yet to find a food for human infants more nutritious than human breast milk. There is solid evidence to support breastfeeding’s benefits to an infant’s immune system. But many of the benefits more commonly cited by advocates—like higher IQ and lower obesity rates—are impossible to disentangle from socioeconomic factors in observational studies, as Brown University economist Emily Oster points out. The few research experiments that have been done on breastfeeding outcomes don’t support the notion that breastfeeding has anything close to a make-or-break impact on child development.
The largest randomized, controlled study of the effects of breastfeeding in the developed world, referred to as the PROBIT trial, began in Belarus in the 1990s. About half of the 17,000 mothers in the trial were randomly selected for a program that promoted breastfeeding and ultimately breastfed their children more; the others were left as a control group. The researchers did find that in this cohort, breastfeeding was correlated with lower rates of diarrhea and eczema in infancy. But Oster’s review of the results, which Quartz confirmed, show that breastfeeding had no discernible impact on outcomes like infant mortality, respiratory infections, obesity, allergies, or IQ.
Another way to get around many of the problems associated with observational studies is to find and compare children who were breastfed to their siblings who were not—in these studies, researchers assume that the parenting experience of the not-breastfed and breastfed child were relatively similar. Like the PROBIT trial, the largest of these studies (pdf), conducted by researchers at Ohio State University, did not find meaningful positive effects of breastfeeding. Using data from an annual survey of American households, the researchers examined health, behavioral, and academic outcomes of siblings between the ages of four and 14, from nearly 700 families where at least one child wasn’t breastfed and one of the others was. They looked at 11 measures of child wellbeing, and found essentially no discernible difference between the breastfed and non-breastfed.
All of this means that breastfeeding is a way to give children a good start in life. It’s just not the only way. “We have good options to provide nutrition to infants that are not just breast milk,” Mirzaian says. “The most important thing is that the child is nourished.”
