More photos from this reportage are featured in Quartz’s new book The Objects that Power the Global Economy. You may not have seen these objects before, but they’ve already changed the way you live. Each chapter examines an object that is driving radical change in the global economy. This is from the chapter on the modafinil, which explores modifying the mind for a more productive life.
People call it “brain zapping” but the correct term is transcranial direct-current stimulation or tDCS. The therapy sends a weak electrical current—a maximum of two milliamps (about a tenth of the current used by a night light)—through the brain to boost or repress neural signals. It’s being heralded by scientists as a possible treatment for a staggering number of neurological issues.
Researchers say it may be a helpful intervention to treat learning disabilities, addiction, obesity, stroke-related speech impairments, age-related cognitive decline, mood disorders like depression, and more. For over a decade, medical researchers have been investigating tDCS as way to treat conditions through neural pathways, while so-called brain hackers and gamers have experimented with it in hopes of gaining a DIY cognitive edge.
Despite all the promise, however, tDCS is in an awkward phase, according to Marom Bikson, a professor of biomedical engineering at The City College of The City University of New York. “It’s among the fastest-growing and most exciting area of treatment in medicine,” he says, but there have not been enough large controlled studies to support all of the headline claims.
“I’m a believer that tDCS can change how we think and feel,” says Bikson, “but scientists still need to be careful about how they promote it.”
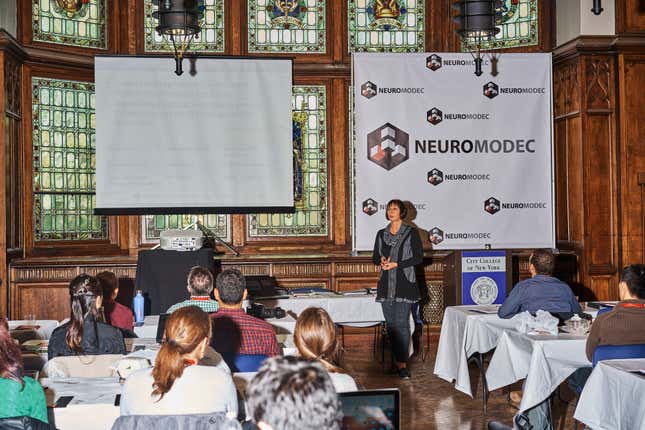
Bikson is considered one of the world’s foremost experts on tDCS. He has been researching its effects in animal models, and later in humans, since 1995, and is currently developing advanced technical devices for medical treatments. Quartz caught up with Bikson in January at the NYC Neuromodulation conference. We asked him about the state of tDCS today.

Quartz: One of the most recent studies on tDCS claimed that it can boost creativity by changing your thought patterns. How does that work?
Bikson: With tDCS, you sometimes deliver energy to a part of the brain to boost its function, or you can deliver energy in way that it disrupts function. The study authors will spell out what their hypothesis is. They will say: We believe that such-and-such area of the brain region is involved in such-and-such function and it’s either a positive or negative relationship, and therefore we apply tDCS to shift the activity of that function in one direction.
So, for example, there may be certain parts of the brain that are exerting a level of control that can in effect clamp down on creativity. You might try to inhibit those brain regions.
It’s just a hypothesis, however. We don’t really understand what brain regions are involved in different functions, especially cognitive functions. Even if tDCS works, it could have worked for some other reason, and even if the effects that are shown in a lab are real, it doesn’t mean that you can do tDCS and then you go do whatever your hobby is and discover that you’re capable of doing things you weren’t capable of doing before.

Of the tDCS findings in the last few years, what are you most excited about?
There was a paper recently in the New England Journal of Medicine: it was a comparison of tDCS and drugs, and the question was: “Is tDCS as good as drugs for depression?” And what they found was that a low dose of tDCS was not as good as a high dose of the drug. But even a low dose of tDCS was better than nothing.
You can see how the media can spin something like that. The main goal was to ask: should a first line of clinical treatment for depression be tDCS? Based on the study, it would suggest maybe not. However the drug also produced significant side effects. Some people might read that paper and incorrectly say it proves that tDCS doesn’t work. But what the study actually showed was that tDCS, as it was applied, was not as good as a high dose of drugs. That doesn’t mean that for some people it didn’t work—because of benefits or side effects—better than drugs.
I found it very exciting because it showed in a controlled trial that tDCS was effective in helping people, but I also find it interesting that it teaches us how nuanced we have to be both running the clinical trials and then discussing the results with the public.
Are there any medical conditions for which tDCS looks particularly promising?
For pain and depression there’s a body of evidence suggesting that tDCS is effective. In many of those cases, the transition to clinical treatment is happening. It’s slow, but it’s happening.
There are also trials that are transitioning [to clinical treatment] for patients with multiple sclerosis to treat cognitive decline. It’s not going to cure MS, but it might improve quality of life for patients. A lot of patients with MS also have a kind of brain fog, and they can also suffer from depression—[for them] tDCS seems to be effective where nothing else is.
Why is it so difficult to explain what’s happening within tDCS with exact science?
That’s not a tDCS problem; that’s a brain problem. We don’t really know how any drug that does something to the brain works. We don’t know what memory is. We don’t know what depression is. Even the things that you think would be easy, like Parkinson’s, we don’t really understand, and it’s the same with age-related cognitive decline. So with tDCS we are treating the black box of the brain, with the limited insight we have on brain function.

There are some clinicians already using tDCS on patients. How are they able to do this when it’s not FDA approved?
The FDA has not approved tDCS for the treatment of any medical condition in the US, but that’s not a negative or positive statement. It’s not that the FDA reads papers and makes decisions. They wait for companies to come to them with a product they want to get approved, and only companies that go through the FDA process can market devices for a specific medical indication.
No tDCS company has yet gone through that process. Because the FDA only regulates medical claims, some companies that are focused on the consumer space, such as tDCS for wellness or exercise, do not approach the FDA. But just because a product does not make medical claims and so is not regulated by the FDA, does not mean is does not need to be built to very high standards.
You can get tDCS across Europe for different indications, and in Singapore and Australia, but not with FDA approval in the US.
There’s also such a thing as off-label treatment, where you can use something that’s not approved. It’s hard to guess how many clinics are using tDCS in the US, but I would put it at under 100.
What are the trends you see developing right now?
For one, there’s a push for bigger clinical trials, and there’s an emphasis on reproducibility. I think another big area is individualizing stimulation, so rather than one-size-fits-all, it’s tailored to individual needs. And then there’s a real push to have these things done at home, with tDCS wearables, rather than having patients come in, which is a real hassle for everyone.
When tDCS is done at home, it can be combined with telemedicine or cognitive training and also wearables. The National Institute of Health is funding work to translate these technologies to home use. Looking forward, this could create a nexus between big data and technology that is directly changing you, and that’s why I am working in collaboration with some [groups] like Google. Digital healthcare, where your health is tracked, and personalized electrical therapy is downloaded to your device, is an area I find very exciting.
Now, a lot of the products that you see on Amazon, you might say “Isn’t that home-based?” Many are cheap versions of devices that were designed to be used in hospitals and labs. The work I’m involved with now is making technology that belongs in this decade; it’s technology that is intended to allow people to change their brain at home.
The results of studies testing whether tDCS can lead to cognitive improvement in healthy people are still mixed. When do you think we’ll know with any certainty whether this form of brain stimulation can provide a cognitive boost for the average healthy brain?
Depending on your standard of evidence, we might be waiting for a while. Look at things like Lumosity brain training. That’s been around a lot longer, and it’s been popular, and now it’s been debunked, but some people swear by it. It’s hard with technology to ever be so conclusive about stuff like mental abilities. Some people already swear by tDCS for helping them function, and some people won’t be satisfied until there’s a massive controlled study.
IARPA [the US military’s Intelligence Advanced Research Projects Activity group] funded large clinical trials, one of which has been published and one that will be [in the future]. These are well-run trials that use hundreds of healthy volunteers and they’re showing that tDCS is able to help some aspects of brain performance like reasoning and problem-solving, but even this more spectacular effort moves the needle only marginally.

I spoke to a clinician who said he could picture a day when everyone will be using tDCS, instead of wine, to relax at the end of the day. What do you think of that?
Yogi Berra said “It’s very hard to make predictions, especially about the future.” I think this scenario is likely, but I can’t say when. Maybe sometime before flying cars, but probably after the iPhone 10.
Having said that, I have no doubt that there are people who are using tDCS that way right now. There’s a whole Reddit section about tDCS. I’m sure for every [tDCS user] on Reddit, there are 100 who are not on Reddit. In principle, I’m having coffee right now, and I’ll have a beer later tonight, and those things are not necessarily any weirder as tools to change how we think and feel as wearing a cap.
Except it’s wearing a cap that’s delivering electricity to your brain.
Wearing a cap with electricity seems weird because it’s not something we’re used to. Who came up with the idea of taking this bean that grows in the wild, grinding it up, and pouring boiling water on it and drinking it? Not applying it to your brain, but drinking it and somehow expecting it to get to your brain. Or taking grapes and letting them rot and bottling that? In this case you’re applying electrical energy directly to the brain to specific parts of the brain that are believed to have a certain function. It’s all relative.
As a scientist I want to share the promise of tDCS but my goal is not to advocate use, by the way. I’m very passionate about people using it to treat suffering. I’m not losing sleep over whether someone is using it to play video games.
Check out Quartz’s new book The Objects that Power the Global Economy.
