One of the tragic features of cancer is that to treat the disease, doctors sometimes have to make the body sicker through chemotherapy. These drugs kill fast-growing cells in the body, like cancer. Unfortunately, a lot of the body’s healthy cells—like those along the digestive tract, hair follicles, and bone marrow—grow quickly, too, and become collateral damage. Simply put, the side effects are horrible: In addition to nausea, vomiting, hair and weight loss, chemo drugs can damage the heart and nervous system, and in rare cases, even cause different types of cancer.
A new study presented yesterday (June 3) at an American Society of Clinical Oncology meeting in Chicago, Illinois, suggests that about half of the women who are diagnosed with a subset of early-stage breast cancer may not need chemotherapy as part of their post-surgery treatment. Instead, these women will likely remain in remission after having their tumors removed, and then taking estrogen-blocking hormone-therapy drugs.
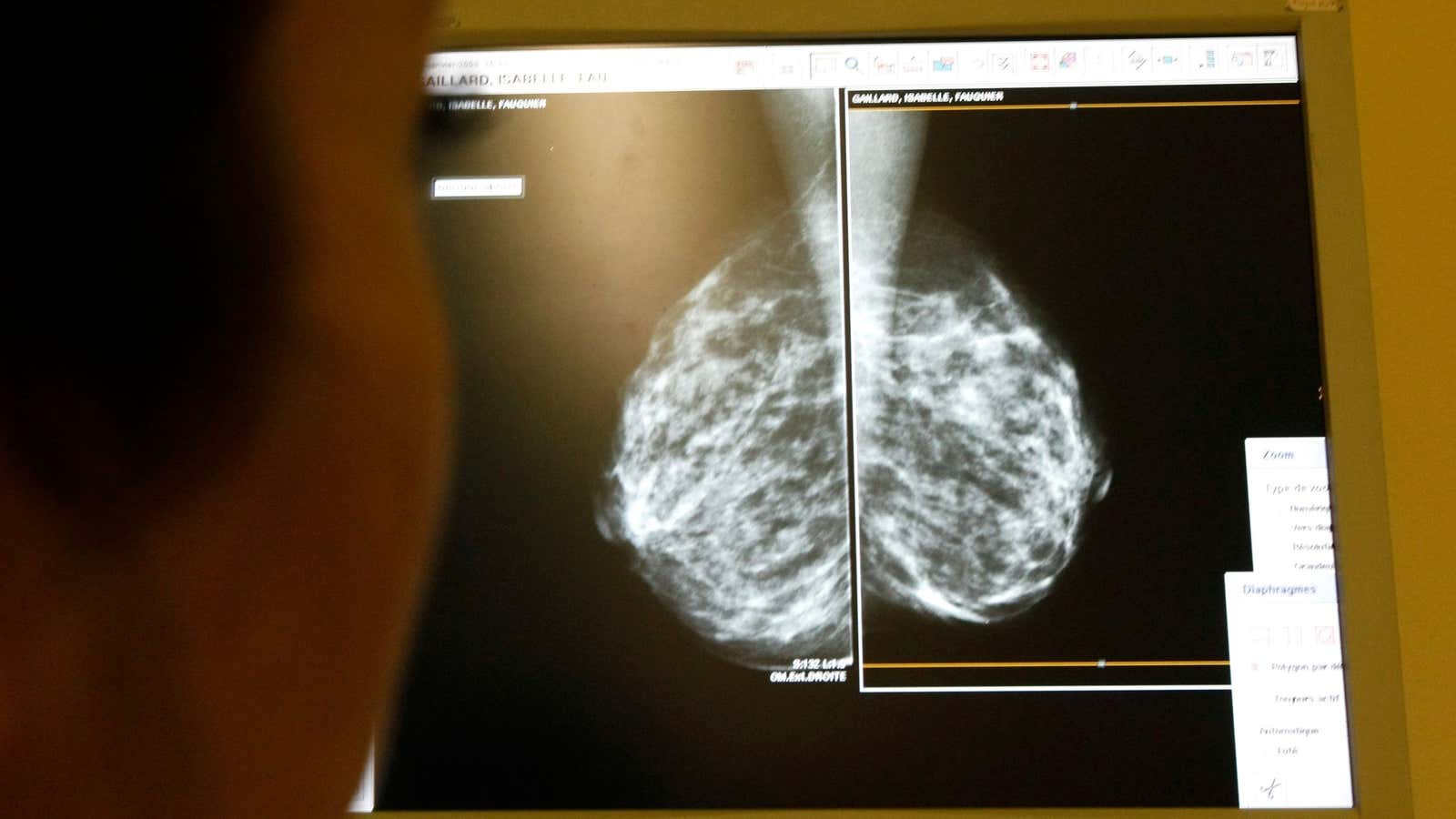
The findings come from a study published simultaneously in the New England Journal of Medicine. The clinical trial followed over 10,000 women with hormone-receptor-positive, HER2-negative breast cancer, that had developed tumors under 5 cm (2 inches) in diameter, and which hadn’t yet spread to the lymph nodes. This characterizes about half of all new breast cancer patients. For context, about 12.4% of women in the US—or about 20 million—will likely develop breast cancer over the course of her lifetime.
In addition to having their tumors removed, the women in the study underwent a genetic test called Oncotype DX, manufactured by California-based Genomic Health. The test looks for 21 specific genes associated with breast-cancer remission. Based on the pattern in which these genes are turned either on or off, the test produces a score between 0 and 100, which measures the woman’s risk of developing breast cancer again in the future.
Doctors allow patients with scores of 10 or below to forgo chemotherapy and take estrogen-blocking drugs alone, because their likelihood of developing recurrent cancer is so low. For patients with scores above 26, doctors always recommend chemotherapy. Patients with scores between 11 and 25, though, represent an uncertainty. Erring on the side of caution, doctors usually give these women chemotherapy.
In this study, almost 7,000 women had scores between 11 and 25. The researchers gave half the women hormone-blocking drugs alone, and half hormone-blocking drugs and chemotherapy. After an average of nine years, 83.3% of those who did not undergo chemotherapy remained cancer-free, compared to 84.3% of those given chemo. This difference is not statically significant.
Chemotherapy did provide some benefit to women in the study who scored between 16 and 25, and were younger than 50 and premenopausal. But of the 7,000 women overall in the 11-25 range, 70% wouldn’t have actually needed chemotherapy, Kathy Albain, an oncologist at Loyola University Medical Center in Illinois, told NPR.
“The uncertainty is over,” she said.
Oncotype DX, the genetic test, costs about $4,000. Most of the time, insurance will cover these costs, and Genomic Health offers a program to help assist those who don’t have adequate insurance.
Although this work does indicate that thousands of women can be spared this difficult treatment, it doesn’t mean skipping chemo is the right choice for all early-stage breast cancer patients. “We must be crystal clear that it applies to a very specific (and significant) subset of women,” Darren Saunders, a cancer biologist at the University of New South Wales in Australia, writes in the Conversation. “Patients should not make any changes to their treatment based off this study, and should always consult their doctors.”