The World Health Organization has issued a grim warning about the fast-growing threat of diseases and infections that no longer respond to the antibiotics and other drugs traditionally used to kill them:
The problem is so serious that it threatens the achievements of modern medicine. A post-antibiotic era—in which common infections and minor injuries can kill—is a very real possibility for the 21stcentury.
In the 129 WHO member countries that participated in the survey, the agency found “very high rates of resistance” to drug treatment in common bacteria like Escherichia coli, Klebsiella pneumoniae and Staphylococcus aureus.
These are bacteria that cause what we think of as unpleasant but completely treatable maladies like bacterial diarrhea, gonorrhea and infected wounds. What’s more, the drugs used against range of microbes, from tuberculosis and influenza to malaria and HIV/AIDS, are growing less effective, the WHO said.
The urinary tract infection, or UTI, is one of most common—more than 50% of women and 5% of men will have one in their lifetime.
Individual countries are now seeing a high incidence of UTIs that aren’t cured with just one round of antibiotics. Recently released research from the UK National Health Services in Scotland shows that more than half of the UTI cases caused by E. coli bacteria that were treated with two of the most common antibiotics (Amoxicillin and Ampicillin) were “anti-microbial resistant,” meaning they couldn’t be cured with those drugs:
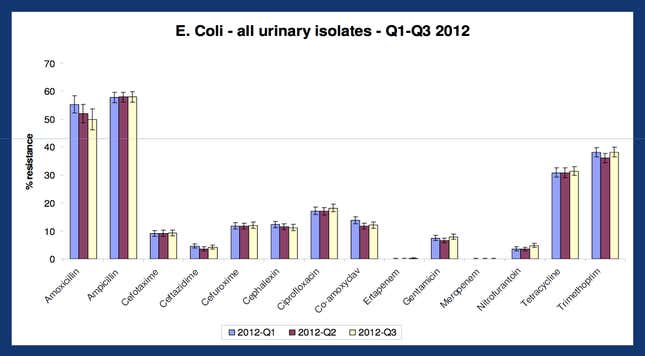
There’s a long list of other drugs that can be used against UTIs, as the chart above shows, so if the first is not successful, another drug is prescribed. But if the infection is not wiped out, it can ultimately spread to the kidneys and other organs, and then to the bloodstream, where it can be fatal.
That’s what often happens to hospitalized patients who die of UTIs. UTIs are the leading “healthcare associated infection,” or infection acquired while in a hospital or a long-term care facility like a nursing home, in high-income countries, the WHO reports. (In low income countries, the most infections from health care come from surgery). Among patients that acquire the infection in US hospitals and facilities like nursing homes, 2.3% die, or some 13,000 a year.
More broadly, drug-resistant diseases and infections are growing in part because of the widespread over-use of antibiotics and other drugs in people and livestock, according to the WHO:
The evolution of resistant strains is a natural phenomenon that occurs when microorganisms replicate themselves erroneously or when resistant traits are exchanged between them. The use and misuse of antimicrobial drugs accelerates the emergence of drug-resistant strains.
Making matters worse, there are no new drugs in development to counter the growing antibiotic-resistant strains of disease. There hasn’t been a single new major antibiotic developed since 1987:
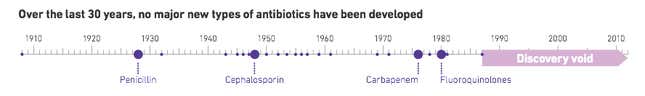
The current round of consolidation in the pharma industry is focused on specialization, creating drug giants that dominate a few areas like oncology or vaccines, but none of these companies are focusing on making new. That’s because these pills historically don’t command a high price and patients only use the drugs for short periods of time, so companies don’t see them as a good business.